Brain Tumors
Adult Tumor Types
Brain tumors often have long, strange names. They may be less confusing once you realize they are named after the type of cell where the primary tumor developed, the location of the tumor, whether it is benign (noncancerous) or malignant (cancerous) and whether it is fast growing (aggressive) or slow glowing. The brain and central nervous system (CNS) are very complex and are made of many different types of cells. Tumors may contain one cell type or can also contain a mixture of cell types.
Research shows that more than 120 types of brain tumors may exist. This section highlights some of the most common brain tumors and their subtypes, where they are located and their notable characteristics.
Gliomas
The most common type of brain tumor is a glioma, which develops from glial cells. These cells are the most common and abundant cell type within the CNS, and they have many functions, including surrounding, protecting and supporting neuron cells with nutrients and oxygen. Any cancer that develops from glial cells is referred to as a glioma, but there are several types of glial cells, including astrocytes, oligodendrocytes and ependymal cells. These tumors are called astrocytomas, oligodendrogliomas and ependymomas.
Astrocytomas
Astrocytes are star-shaped cells that compose the supportive tissue of the brain. Astrocytomas begin in astrocytes and make up the majority of gliomas. They can develop in various parts of the brain and CNS, including the cerebellum (back part of the brain), the cerebrum (large front portion of the brain), and central areas of the brain, brain stem and spinal cord.
Astrocytomas may be difficult to remove surgically because they spread widely throughout the brain and infiltrate and blend into normal brain tissue. In some cases, they spread along the cerebrospinal fluid (CSF) pathways, but they rarely spread outside of the brain or spinal cord.
Astrocytomas are graded on a scale from I to IV based on how abnormal the cells look under a microscope. Low-grade astrocytomas are typically contained in one location and grow slowly. High-grade astrocytomas grow rapidly, spread into surrounding tissues and are typically found in adults.
Following are the most common types of astrocytomas, from low grade to high grade.
Pilocytic astrocytomas are typically classified as Grade I. They are considered the most benign (noncancerous) of all of the astrocytomas. They tend to stay in the location where they begin and do not spread. Although they are usually slow growing, these tumors can become very large.
Diffuse astrocytomas, also known as astrocytoma Grade II, are low grade. With Grade II, more cells look abnormal when examined under a microscope than with Grade I. The tumors can spread to nearby tissues but are more likely to invade surrounding tissue than a Grade I tumor. They tend to grow at a relatively slow pace. They typically contain the IDH and 1p/19q molecular markers.
Anaplastic astrocytomas are considered Grade III tumors and are fairly rare. They are malignant and often require more aggressive treatment than pilocytic and diffuse astrocytomas. Anaplastic astrocytomas may develop in any area of the CNS but are more likely to begin in the cerebrum, including any of the lobes (frontal, temporal, parietal or occipital). Other common sites for anaplastic astrocytomas include the part of the brain that contains the thalamus and hypothalamus, the lower area of the brain near the back of the neck that controls movement and balance (cerebellum) and the spinal cord. These tumors tend to have tentacle-like projections that grow into surrounding tissue, making them difficult to completely remove during surgery.

Glioblastomas are considered high-grade tumors (Grade IV). They are also known as astrocytoma Grade IV or glioblastoma multiforme (GBM) because the cells may take a variety of appearances under the microscope. There are two types of glioblastoma — primary and secondary. Primary tumors are very aggressive and are the most common form of astrocytoma Grade IV. Secondary tumors begin as lower-grade tumors and evolve into Grade IV tumors.
Glioblastomas usually contain a mix of cell types. They increase in frequency with age and affect more men than women. They have finger-like tentacles and single cells that can migrate long distances, and they are difficult to completely remove, particularly when they are near parts of the brain that control functions such as language and coordination.
Although glioblastomas can be found anywhere in the brain or spinal cord, they are generally found in the cerebral hemispheres of the brain. They are usually highly malignant (cancerous) because the cells reproduce quickly and migrate into the brain substance, and they are supported by a large network of blood vessels. These cells are able to easily invade and live within normal brain tissue. However, they rarely spread elsewhere in the body.
Oligodendrogliomas
These tumors develop from fried-egg-shaped cells called oligodendrocytes. Oligodendrogliomas, which contain the IDH and 1p/19q molecular markers, are classified as oligodendrogliomas and anaplastic oligodendrogliomas.
Oligodendrogliomas are considered low grade (Grade II). Because of their generally slow growth, they often are present for years before they are diagnosed.
Anaplastic oligodendrogliomas are malignant and more aggressive (Grade III).
The frontal and temporal lobes are the most common locations for these tumors, but they can be found anywhere within the cerebral hemisphere of the brain. Tumors typically appear soft and grayish-pink, and they often contain mineral deposits (calcifications), areas of hemorrhage (bleeding) and/or cysts.
Ependymomas
Ependymomas develop from ependymal cells, which line the ventricles of the brain and the middle of the spinal cord. The ventricles are the passageways where cerebrospinal fluid is made and stored. These tumors range from low grade, which are less aggressive, to high grade, which are more aggressive.
Ependymomas can be either Grade I or II, are less aggressive and typically grow slowly with mostly normal cells when viewed under a microscope. They usually are located along, within or next to the ventricular system. Grade I ependymomas can be either myxopapillary ependymomas or subependymomas. Grade II ependymomas grow into the ventricles.
Anaplastic ependymomas grow quickly and may spread into surrounding tissues. When viewed under a microscope, the cells look different than normal cells. This type is rarely found in the spinal cord.
Because ependymomas form in the cells that line the ventricles, they most often spread along the cerebrospinal fluid pathways but rarely spread outside the brain or spinal cord. They are typically soft and grayish or red and may prevent cerebrospinal fluid from leaving the ventricles, which causes the ventricles to enlarge.

Meningiomas
The most common primary brain tumor in adults, meningiomas develop in the meninges, which consist of three layers of tissue that cover the outer part of the brain inside the skull and spinal cord. Because the meninges surround the brain, meningiomas are usually found in the layers on the top of the brain and the outer curve. They may form at the base of the skull as well.
Meningiomas sometimes occur in families who have neurofibromatosis, a genetic syndrome in which many benign tumors of nerve tissue develop. These tumors are more likely to be found in adults older than 60, and the incidence appears to increase with age.
The majority of meningiomas are benign (noncancerous), but some may be classified as malignant (cancerous). Although rare, malignant meningiomas may be highly aggressive. Even if the meningioma is benign, it can cause problems if it grows into nearby areas of the brain. These tumors typically grow slowly and inward, putting pressure on the brain or spinal cord, which can interfere with normal brain function. However, they also can grow outward toward the skull and cause it to thicken. Some contain sacs of fluid (cysts), mineral deposits (calcifications) or tightly packed bunches of blood vessels.
These tumors are graded from Grade I to Grade III. Grade I meningiomas are benign and look mostly normal under a microscope. Grade II meningiomas may be considered atypical or invasive, and the cells look more abnormal than Grade I tumors. These can grow beyond the meninges and into the brain’s tissues. Grade III meningiomas may be considered anaplastic or malignant and look mostly abnormal under a microscope. These grow quickly, can grow into other parts of the brain and bone, and can return after treatment.
It is estimated that a majority of meningiomas contain an abnormal chromosome 22 that typically suppresses tumor growth. The exact cause of this abnormality is unknown. Research has found that meningiomas typically have extra copies of the platelet-derived growth factor (PDGF) and its receptor (PDGFR) and epidermal growth factor receptor (EGFR) genes, which may cause these tumors to grow. This may be the subject of further research in clinical trials.
Choroid Plexus Tumors
The choroid plexus is a network of blood vessels and cells in the ventricles (fluid-filled spaces) of the brain. The blood vessels are covered by a thin layer of cells that make cerebrospinal fluid. Choroid plexus tumors are rare and can develop in both children and adults, but are more common in children. These tumors mostly form inside the ventricles, but may also be found in other regions of the CNS, and may have a “cauliflower-like” appearance on imaging tests.
The majority of choroid plexus tumors are benign (non-cancerous) but can sometimes become malignant (cancerous). They are grouped into three grades based on how fast the cells are growing.
Choroid plexus papillomas are considered Grade I and mostly benign. The cells grow slowly and rarely spread to other parts of the brain or spinal cord. They represent the majority of all choroid plexus tumors.
Atypical choroid plexus papillomas are considered Grade II and are more likely to return after surgery.
Choroid plexus carcinomas are considered Grade III and are the rarest of the choroid plexus tumors. They are malignant. The cells are fast growing and may spread to other nearby tissues.
When these tumors form, they can cause an overproduction of cerebrospinal fluid. The tumor can cause fluid buildup and/or press on the brain, resulting in nausea, vomiting, headaches, extreme fatigue, blurred or double vision, seizures or hearing loss. Although some genetic changes have been associated with these tumors, their cause is still unknown.
Pineal Gland Tumors
The pineal gland is a small endocrine gland that sits between the cerebral hemispheres. It makes melatonin, a hormone that regulates sleep, in response to changes in light. The pineal gland is located inside the brain, yet it is not considered part of the brain. A tumor that develops in this area often affects other areas of the brain that surround this gland.
Tumors in the pineal region are rare. Although they typically remain confined to the pineal gland and nearby tissues, a small percentage of the tumors, particularly pineoblastomas, can potentially spread through the cerebrospinal fluid. When this occurs, it is typically late in the disease.
Pineocytomas are considered Grade I or II, are less aggressive and typically grow slowly with mostly normal cells when viewed under a microscope. They can be relatively benign.
Pineal astrocytomas can be any grade and form in the tissue surrounding the pineal gland.
Pineal parenchymal tumors of intermediate differentiation are considered Grade II or III and fall between pineocytomas and pineoblastomas, which are Grade IV. Parenchymal cells (pineocytes) are the cells that make up most of the pineal gland. The tumor cells may spread into nearby tissue or the cerebral spinal fluid. These cells look very different under a microscope.
Papillary tumors of the pineal region are relatively uncommon and have only recently been recognized by the World Health Organization. They do not develop within the pineal gland but, instead, may grow from regions or structures around the pineal gland. Grades have yet to be determined for this group, but it is believed they are close to Grade II or III.
Pineoblastomas are Grade IV, malignant (cancerous) and the most aggressive. Their cells look very different under a microscope, and their cells may even contain dead regions. They may resemble medulloblastomas and retinoblastomas.
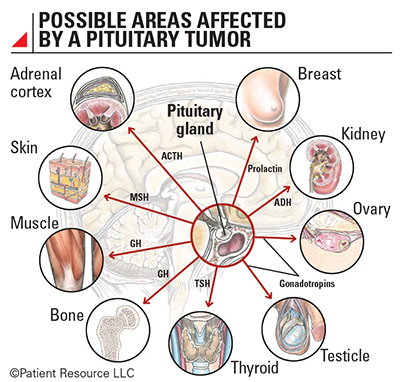
Pituitary Tumors
The pituitary is a small gland located inside the brain. It sits above the nasal passages, which are above the fleshy back part of the roof of the mouth (known as the soft palate). The pituitary gland is responsible for releasing multiple types of hormones that affect many bodily functions. Sometimes referred to as the “master endocrine gland,” it produces hormones for the thyroid, adrenal gland, testicles, ovaries and breasts as well as melanin, oxytocin and growth hormones.
Two types of tumors start in the pituitary gland.
Pituitary adenomas are divided into benign pituitary adenomas and invasive pituitary adenomas. Benign pituitary adenomas grow very slowly and do not spread outside of the pituitary gland. However, invasive pituitary adenomas may spread to the skull or the sinus cavity below the pituitary gland.
Pituitary carcinomas, also known as pituitary cancer, are malignant (cancerous) and are very rare. They can grow into other areas of the brain and spinal cord or outside of the CNS.
Almost all pituitary tumors are pituitary adenomas, which are benign. However, they still can cause problems if they grow large enough to press on nearby structures or if they make too much of any kind of hormone. For example, optic nerves that send visual information from the eyes to the brain are near the pituitary gland and may be affected by a tumor in this region.
Pituitary tumors can occur at any age, but they are most often found in older adults. The majority of pituitary adenomas develop in the front two-thirds of the pituitary gland.
Along with being considered benign or malignant, the tumors may be classified as “functioning” or “non-functioning” because the pituitary gland connects the brain with the endocrine system, which is responsible for directing the body to make hormones. Most pituitary tumors are the “functioning” type, producing larger than normal amounts of one or more hormones.
When pituitary tumors grow outside of the gland, they have very little room to grow in this part of the skull. Therefore, if they become larger than about 1 cm (about half an inch) across, they may grow upward where they can compress and damage nearby parts of the brain and the nerves that arise from it, especially vision.
Schwannomas
Schwannomas are tumors that form in Schwann cells, which primarily cover and protect cranial nerves, but can include other nerves as well. Although they can form on any cranial nerve, they typically develop on the vestibulocochlear nerve, which is near the cerebellum and controls hearing and balance. In this case, they are called vestibular schwannomas or acoustic neuromas. Schwannomas can also begin on spinal nerves where they extend from the spinal cord. When they press on the spinal cord, they can cause weakness, sensory loss, and bowel and bladder problems.
Schwannomas are almost always benign and usually very slow growing. They are considered Grade I tumors. The vast majority of them occur spontaneously and as a single tumor. Multiple schwannomas may develop in a small percentage of people and may be due to an inherited condition that was passed from parent to child.
| Other Types of Brain Tumors Found in Children & Adults* | |
| Diffuse astrocytic and oligodendroglial tumors |
Gemistocytic astrocytoma
Giant cell glioblastoma Gliosarcoma Epithelioid glioblastoma Diffuse midline glioma |
| Other astrocytic tumors | Anaplastic pleomorphic xanthoastrocytoma |
| Ependymal tumors |
Papillary ependymoma
Clear cell ependymoma Tanycytic ependymoma |
| Other gliomas | Astroblastoma |
| Neuronal and mixed neuronal-glial tumors | Anaplastic ganglioglioma |
| Tumors of the cranial and paraspinal nerves |
Malignant peripheral nerve sheath tumor (MPNST)
Epithelioid MPNST MPNST with perineural differentiation |
| Meningiomas |
Papillary meningioma
Rhabdoid meningioma Anaplastic (malignant) meningioma |
| Mesenchymal, nonmeningothelial tumors |
Solitary fibrous tumor/hemangiopericytoma
Epithelioid hemangioendothelioma Angiosarcoma Kaposi sarcoma Ewing sarcoma/peripheral primitive neuroectodermal tumor Liposarcoma Fibrosarcoma Undifferentiated pleomorphic sarcoma/malignant fibrous histiocytoma Leiomyosarcoma Rhabdomyosarcoma Chondrosarcoma Osteosarcoma |
| Melanocytic lesions |
Meningeal melanoma
Meningeal melanomatosis |
| Lymphomas |
Diffuse large B-cell lymphoma of the CNS
Anaplastic large cell lymphoma Intravascular large B-cell lymphoma MALT lymphoma of the dura |
| Histiocytic tumors |
Langerhans cell histiocytosis
Erdheim-Chester disease Histiocytic sarcoma |