Breast Cancer
Treatment Options
Though you may be familiar with many of the general therapies that treat breast cancer, knowing the treatments available for your unique diagnosis will help you feel more in control. New advances continue to be introduced, offering more hope for cure and more ways to improve the quality of life for people who are living with advanced breast cancer.
You and your doctor will plan your treatment together. To personalize your plan, your doctor will take into account your age, general health and menopausal status, as well as the size of the tumor, its biomarker status (ER, PR, HER2), the stage of the cancer and genetic markers, such as BRCA1 (breast cancer 1) and BRCA2 (breast cancer 2) mutations, if applicable. You will provide input about things that are important to you, such as your expectations for your quality of life. Then, together, you will define your treatment goals.
Your doctor may adjust or change your treatment if your cancer becomes resistant (stops responding) to any of the drug therapies or if your cancer recurs after previous treatment. You are encouraged to stay informed about the treatments that are available should your cancer stop responding. When you know your options, you will be ready to pivot if the situation calls for it. It is much easier to make a confident decision when you are not rushed or panicked.
About Cancer Treatment
Your treatments will be either local or systemic. Local treatments target specific areas of the body and include surgery and radiation therapy. Systemic treatments include drug therapies (targeted therapy, chemotherapy, immunotherapy and hormone therapy) that travel throughout your body. Drug therapies can be given orally or intravenously (IV) through a vein in your arm or through a port. A port is surgically inserted under the skin in the upper chest area or arm to gain easy access to veins.
Whether delivered before or after surgery, an important goal of systemic therapy is to destroy breast cancer cells that may be hiding in other organs of the body, such as the liver, lungs, bones or brain. These hidden cancer cells, called micrometastatic disease, are usually too small to detect with laboratory testing or imaging studies. Delivering carefully selected systemic therapy to appropriate patients can often completely eliminate micrometastatic disease and is, therefore, extremely important as a partner with surgery for breast cancer in helping a patient become disease-free.
Your doctor will consider your age, general health and menopausal status for women, as well as the size of the tumor, its biomarker status (ER, PR, HER2), the stage of the cancer and genetic markers, such as BRCA1 and BRCA2 mutations, if applicable, and the results of genomic testing. It is important to share your expectations for your quality of life. Then, together, you and your doctor will define your treatment goals.
Your doctor may adjust your treatment if the cancer becomes resistant (stops responding) to your current drug therapy or if the cancer recurs after previous treatment.
Following are common treatment options that may be used alone or in combination.
Surgery is the most common treatment for most breast cancers. It removes the tumor in the breast and it may be used to prevent or treat symptoms or complications of breast cancers that have metastasized to distant organs.
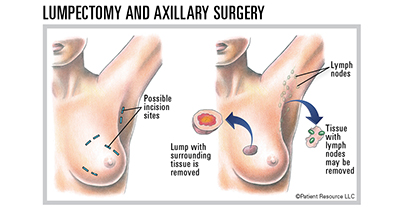
Lymph node surgery is usually necessary to stage the cancer (called a sentinel lymph node biopsy) or to control cancer that has spread to the nodes. The underarm (axilla) is the most common site of spread for breast cancer.
A lumpectomy, also called breast-sparing or breast-conserving surgery, removes the tumor along with a small margin of normal-appearing tissue around it. It is used for early-stage breast cancers detected as small tumors. A lumpectomy is usually followed by radiation treatments, which are designed to kill microscopic cancer cells hiding in other parts of the breast.
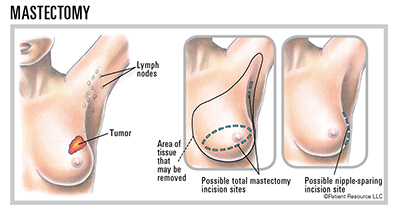
A mastectomy involves removal of the entire breast. Total mastectomy is the surgical removal of the entire breast without removing muscle. In a modified radical mastectomy, a total mastectomy is performed along with removal of a block of underarm (axillary) lymph node tissue (axillary dissection). Drains may be placed to collect fluid and assist in healing. Reconstructive surgery may be an option.
Survival rates for breast-conserving surgery plus radiation therapy compared to total mastectomy (with or without reconstruction) are essentially the same. Ongoing follow-ups after both types of surgery are important and recommended.
Radiation Therapy
Radiation therapy is almost always delivered after lumpectomy to destroy cancer cells that may be hidden in normal-appearing breast tissue. Research shows that a person with a small tumor who has radiation therapy after a lumpectomy has similar survival rates and risk of recurrence as someone who has a mastectomy.
Post-mastectomy radiation therapy is sometimes necessary. For those patients with a high risk of the cancer growing back on the chest wall area (after mastectomy and/or axillary surgery), radiation can lower this risk. Radiation therapy may also be used for people who have metastatic breast cancer to control symptoms from specific areas of cancer involvement, such as bone or brain metastases.
The most common type of radiation therapy is external-beam radiation therapy (EBRT). EBRT is delivered from an external machine. Internal radiation, or brachytherapy, may also be used either alone or in combination with EBRT for lumpectomy patients. Brachytherapy involves placing radioactive seeds through a catheter into the breast to deliver radiation directly to the area where the tumor was removed.
Drug Therapy
Chemotherapy drugs may be used as neoadjuvant (preoperative) therapy to shrink a large, bulky tumor so it can be removed surgically or to reduce the tumor’s size to offer more surgical options. Neoadjuvant chemotherapy also offers the advantage of helping your doctor determine how well the chemotherapy drugs work against the tumor, and to identify whether additional therapy is needed post-operatively. Adjuvant (after surgery) chemotherapy is given to destroy cancer cells that may remain in the body.
Targeted therapy uses drugs or other substances to identify, attack and destroy specific types of cancer cells or to slow disease progression. Types include anti-HER2 drugs, kinase inhibitors and monoclonal antibodies. It can be given before or after surgery.
Hormone therapy is used to treat ER+/PR+ tumors. Several types may be used depending on the stage of the cancer and menopausal status of the female patient. Drugs that lower or block estrogen may be used, or the ovaries may be removed with surgery or suppressed with medication or radiation therapy.
Immunotherapy is designed to stimulate the body’s own immune system to treat certain breast cancers.
Clinical trials may be another option.
Clinical Trials
Clinical trials are medical research studies that may offer access to leading-edge treatments not yet widely available. Sometimes a clinical trial may be the best treatment option when an individual’s cancer has become resistant to the current treatment; when curative therapies are not yet available for that cancer type, subtype or stage; or the cancer is rare and has few, if any, approved treatments. Ask your doctor if you should consider this valuable option. Learn more about clinical trials here
Medication Adherence
Oral cancer therapies that can be taken at home in pill form offer many benefits: convenience, fewer appointments, no transportation or parking issues and no needle sticks. Though oral therapies offer great convenience, they also put the responsibility on you for taking them exactly the way your doctor instructs. Taking the right drug in the right dose at the right time for as long as prescribed is referred to as medication adherence.
Even with the best intentions, adherence can be challenging, especially if you are taking multiple medications on different schedules. Set yourself up to succeed by making sure you fully understand instructions for how and when to take your medications. Track each dose, including missed doses, and detail any side effects. Many medication reminders and organizers are available. These range from setting an alarm clock or a phone alarm to wearing a vibrating wristwatch or downloading a smartphone app.
You may be tempted to stop taking your oral therapy to avoid uncomfortable side effects or save money, but even small changes to your regimen can disrupt your treatment and affect its outcome. Most cancer therapies are designed to maintain a specific level of drugs in your system for a certain time based on your cancer type and stage, your overall health, previous therapies and other factors. Don’t stop taking your medications or alter your dosage without talking to your doctor or your health care team.
| Commonly Used Medications |
| Chemotherapy |
|
| Hormone Therapy |
|
| Immunotherapy |
|
| Targeted Therapy |
|
| Some Possible Combinations |
|
Reconstruction: Post-Surgical Options
Your decision regarding breast reconstruction is one only you can make. Your breasts may play a crucial role in your personal sense of femininity and sexuality. You may be eager to replace them to feel more like your pre-cancer self. If so, consider reconstructive surgery or prostheses. Or you may prefer what’s referred to as “going flat,” which means not having a breast prosthesis, enhancement or additional surgery. Before you make this highly personal choice, learn as much as you can about your options and think about what will make you most comfortable.
If you are having a mastectomy or lumpectomy, your doctor will likely discuss breast reconstruction, which involves additional surgeries to restore or reshape one or both breasts. Reconstructive surgery is often performed, or at least started, during a mastectomy or can be delayed for a few months or even years. It may be done during or after a lumpectomy if the surgery will cause the affected breast to look significantly different from the other after the tumor is removed.
Flap reconstruction involves recreating the breast using a flap of tissue, usually with skin, fat, possibly muscle and blood vessels from elsewhere in your body. Various techniques are available depending on the tumor’s size and location, size of your breasts, your body type, whether your breast has been radiated in the past and your preferences. Flap procedures should be performed by an experienced plastic surgeon who specializes in breast reconstruction.
Implant-based reconstruction, using silicone or saline implants, initially requires less extensive surgery than tissue flap procedures. The overlying chest wall muscle and skin may be stretched by inserting a tissue expander under the muscle to accommodate the implant. The expander is gradually inflated with fluid injections through the skin until the desired size is reached. In some cases, the implant is placed on top of the chest wall muscle but underneath the skin. When the tissue expander is inflated to the proper size, the plastic surgeon will arrange for a follow-up “exchange” surgical procedure that replaces the tissue expander with the final implant. Some patients will be candidates for a single-stage, direct-to-implant reconstruction performed at the time of the mastectomy.
Non-surgical options, such as a breast prosthesis, are also available. Made from artificial materials, the prosthesis is designed to provide a natural, symmetrical appearance when you’re dressed. You must wait until you’re healed from surgery to be fitted for a prosthesis. One type is worn inside the hidden pocket of a mastectomy bra. Another type attaches to your body with a special adhesive, though this approach may not be recommended after chest wall radiation therapy.
Mastectomy bras are available in many styles and colors. Many health insurance providers will cover the costs of a prosthesis and mastectomy bras if you provide a prescription from your oncologist or oncology surgeon. Call your insurer beforehand to verify which mastectomy-related products are covered, documentation required for reimbursement and how often you can purchase replacements.
As you explore your options, consider:
- Breasts are not essential organs for life, though you may feel they are integral to your identity as a woman.
- Your plastic surgeon will work with you to set expectations for what your new or reconstructed breast(s) will look like. Keep in mind that even with reconstruction, your breast(s) will not look or feel exactly as they did before or have the same sensation.
- Many advocacy groups offer peer counseling, so you can ask questions of women who’ve had reconstruction procedures. Ask your nurse/patient navigator for referrals.
Reconstruction: Post-Surgical Options
With an Implant A breast implant filled with silicone gel or saline (salt water) may sometimes be placed following the mastectomy in a single operation referred to as immediate reconstruction. In delayed reconstruction, a tissue expander is inserted under the skin following the mastectomy to gradually stretch the skin and underlying tissue; an implant is then placed in a second surgery, often when treatment is completed.
With a Tissue "FLAP" A tissue “flap” usually contains skin, fat, blood vessels and sometimes muscle. A pedicle flap remains attached to the body and is repositioned to the breast area with a muscle carrying the blood supply. A free flap is removed from the body along with blood vessels, which are then attached to the blood vessels in the breast area. Some types of flaps follow.
[DIEP] deep inferior epigastric perforator flap
[SIEA] superficial inferior epigastric artery flap
[TRAM] transverse rectus abdominis muscle flap
[LD] latissimus dorsi flap
[GAP] gluteal artery perforator flap (gluteal free flap)
[SGAP] superior gluteal artery perforator flap
[PAP] profunda artery perforator flap
[TUG] transverse upper gracilis flap