Fertility Issues
Parenthood is something you may envision for yourself, and cancer and its treatments can sidetrack your path to getting there. Age and overall health also play a role in your fertility. Because fertility issues often arise as soon as treatment begins, it is essential to talk to your oncologist and a fertility specialist before beginning treatment. Options for preserving your fertility become much more limited after treatment starts.
Because the causes of cancer-related fertility issues and ways to manage them differ for women and men, this information is explained by gender.
Females: For a woman to become pregnant naturally after cancer treatment, she must have at least one healthy ovary to produce the egg, one healthy fallopian tube through which the egg travels, a healthy uterus for the baby to grow, and correct levels of certain hormones that help maintain the pregnancy. An absence or imbalance of any these factors can lead to fertility problems after cancer treatment.
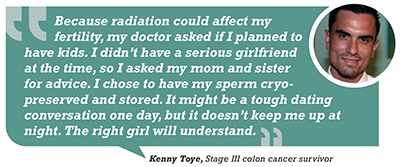
Males: Men who are unable to produce or ejaculate healthy sperm are technically considered to be infertile. This can happen for a number of reasons and can often be a result of different types of cancer treatment.
What causes fertility issues?
Many conditions during cancer treatment can affect fertility after treatment ends. Drug therapies, radiation therapy and surgery can cause fertility issues. The endocrine glands and related organs release hormones that control fertility. When cancer or cancer treatments, such as certain drug therapies, surgery or radiation therapy, damage one of these glands or organs, or alter the area of the brain that controls the endocrine system, challenges with fertility can occur.
Females: In some cases, the effects of some therapies may be reversible, with function returning gradually over a few months or even years after treatment has ended. Ovarian shielding (placing external shields over your ovaries during radiation therapy to minimize exposure and damage) and ovarian suppression (taking a medication that causes the ovaries to temporarily shut down during chemotherapy) may be options. In contrast, loss of function is permanent when reproductive organs are surgically removed.
Males: The effects of some cancer treatments on the testicles can sometimes be reversible, although it isn’t typical. Regaining full sexual function after treatment may take time, mostly because both psychological and physical factors are involved. Loss of function is permanent if these organs have been surgically removed or altered.
How you can manage fertility issues
Ask about the risk of fertility issues from each type of treatment you are considering. Also ask about preventive measures that are available. Making your treatment team aware of your life goals, such as becoming a parent or expanding your family, is very important and needs to be discussed before any treatments are started or even considered.
Addressing the emotions that come with fertility problems resulting from cancer and treatment is good for both you and your partner. Keep the lines of communication open as well, which will help you to understand what’s important to each of you while making these important decisions. Consider counseling (individual, couples and/or sex therapy) and physical exercise, which can help lower your stress surrounding this situation. You may also find it helpful to talk with a spiritual advisor.
Adoption is another option that lets you legally accept the responsibility for a child. Get in touch with an adoption attorney or agency to learn more, especially because some agencies are more open than others when working with cancer survivors.
Females: Your health care provider may be able to prescribe medication to help stimulate ovulation; however, this type of treatment is usually only beneficial to women whose infertility is due to problems with ovulation.
Learn more about the fertility alternatives that are available, including assisted reproductive technologies (ART), such as intrauterine insemination (IUI), in vitro fertilization and third-party-assisted ART. If you were unable to preserve your fertility before treatment, third-party-assisted ART may be an option. This involves the use of sperm donors, egg donors and/or surrogates.
A combination of treatments may be your best option. You may be able to use in vitro fertilization with donor eggs or have your frozen embryos carried to term using a surrogate. Talk to a fertility specialist about the options available to you.
Males: If you didn’t pursue the use of sperm banks, testicular sperm extraction or gonadal shielding prior to radiation therapy, little can be done to reverse the effects afterward.
Donor insemination is a possibility that allows you to use someone’s sperm that you know (such as a friend or relative) or the sperm of a random donor. The semen is then used to create a pregnancy via intrauterine insemination (IUI).
When to call your health care provider about fertility issues
From the start, as you consider your treatment options, see a fertility specialist to determine whether you are fertile and what precautions you can take to help preserve your fertility. Your health care provider should be able to give you a referral.
Regardless of whether you were able to take precautions before beginning treatment, if you and your partner have been actively trying to conceive for a year after treatment ends but have been unsuccessful, ask your health care provider or fertility specialist for referrals to help you explore other possibilities.