Head & Neck
Oral Cancer
Includes illustrated staging details
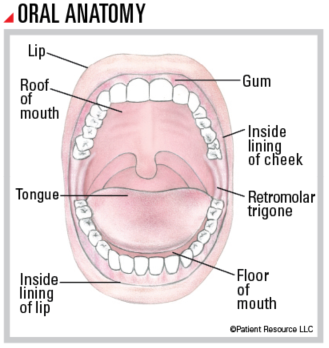
More than half of all head and neck cancers develop in the oral cavity (also called the mouth), which includes the lips, gums, lining inside the cheeks, roof of the mouth, retromolar trigone (small spot behind the wisdom teeth), front two-thirds of the tongue, and the floor of the mouth underneath the tongue. Most oral cancers form from squamous (SKWAY-mus) cells, which are thin, flat cells that line moist surfaces in your mouth and throat.
The symptoms of oral cancer can also signal many other conditions, so they are frequently diagnosed at a late stage. Some symptoms may include a sore in the mouth or lip that doesn’t heal; red or white patch on the gums, tongue, tonsil or lining of the mouth; a lump on the lip, mouth, neck or throat; persistent sore throat; hoarseness or change in voice; and difficulty chewing, swallowing or moving the jaws or tongue. Dentists typically screen for cancer at regular six month or annual appointments.
Treatment Options
When discussing your treatment plan with your doctor, keep in mind that your ability to speak and eat normally and your appearance may be altered. As a result, it is very important to have detailed discussions with your doctor about the benefits, risks and potential side effects and late effects of every treatment, including quality-of-life issues. You are also encouraged to discuss reconstructive options. Many surgeons who remove head and neck cancer are also trained in reconstruction and can expertly perform both parts of the surgery (see Reconstruction & Rehabilitation).
Your treatment plan may include one or more of the following options.
Surgery is typically the recommended treatment for oral cavity cancers. It is performed to remove small, early-stage tumors of the lip, gums, roof of the mouth, front of the tongue, floor of the mouth and inside the cheeks. It may also be used to remove larger tumors and those that have metastasized (spread) to nearby tissue or lymph nodes in the neck. The goal of surgery is to remove the tumor; however, your surgeon will also focus on preserving as much function as possible. Various procedures and techniques are potential options.
Tumor resection removes the tumor and a margin of healthy tissue surrounding it.
Glossectomy removes all or part of the tongue. A partial glossectomy removes less than half of the tongue; a hemiglossectomy removes half of the tongue; and a subtotal or total glossectomy removes most or all of the tongue.
Maxillectomy removes all or part of the hard palate.
Mandibulectomy removes all or part of the jawbone.
Composite resection is common in treating advanced oral cancers. It may involve the removal of multiple areas affected by cancer, such as part of the jaw, tongue and floor of the mouth.
Mohs micrographic surgery may be recommended for some types of lip cancer. After removing the tumor, the surgeon removes a tiny fragment of tissue that had surrounded it and examines it under a microscope. The process is repeated until clear margins are seen. This type of procedure is performed by a dermatologist.
Neck dissection removes some of the lymph nodes in the neck when the cancer has spread to the area, or if there is a significant risk it will spread to the lymph nodes.
Reconstructive procedures may be recommended to repair or replace removed areas, improve the ability to eat and speak, and help restore appearance as much as possible (see Reconstruction & Rehabilitation).
Radiation therapy may be recommended if you are not a candidate for surgery (due to other medical problems or the extent of the cancer). It is not designed to cure the cancer, but to slow down its growth and spread, and alleviate symptoms.
When it is used, it is given after surgery as adjuvant therapy to destroy remaining cancer cells and reduce the risk of the cancer recurring. It may also be used alone or with chemotherapy (chemoradiation) for cancer that has a high risk of recurring. It can be given in the form of external-beam radiation therapy, which is delivered by a machine outside of the body.
Radiation therapy to the oral cavity can affect your teeth. Before beginning this type of treatment, you will be required to have a thorough dental exam with a dentist experienced in treating people with cancer to address existing problems (see Dental & Oral Side Effects). If you smoke, be aware that research indicates radiation therapy is more effective in patients who have stopped smoking before beginning treatment.
Drug therapy may be used alone or with other therapies.
Chemotherapy can be used for oral cavity cancer if you are not a candidate for surgery. This can be given with the goal of slowing down the growth and spread of the cancer. It is more commonly used as adjuvant treatment following surgery if your cancer has aggressive features and a high risk of returning.
Immunotherapy in the form of immune checkpoint inhibitors may be part of your treatment plan if you have recurrent or metastatic oral cancer. The doctor will test for the tumor’s PD-L1 expression, which may indicate whether the tumor could respond to immunotherapy. If expression is more than 1 percent, the tumor is considered to be PD-L1 positive and immunotherapy alone may be used. If
PD-L1 is negative, immunotherapy and traditional chemotherapy are often combined for patients who have recurrent or metastatic cancer.
Targeted therapy may be an option to treat types of oral cancer that contain specific genetic abnormalities, proteins or growth factors. Targeted therapy in the form of epidermal growth factor receptor (EGFR) inhibitors may be used in combination with radiation therapy. Targeted therapy drugs may be given alone or in combination with chemotherapy or radiation therapy.
TNM Classification for Oral Cancer
| Classification | Definition |
| Tumor (T) | |
| TX | Primary tumor cannot be assessed. |
| Tis | Carcinoma in situ. |
| T1 | Tumor not more than 2 cm, with depth of invasion (DOI) not more than 5 mm. DOI is depth of invasion and not tumor thickness. |
| T2 |
Tumor not more than 2 cm, with DOI more than 5 mm
or tumor more than 2 cm but not more than 4 cm, with DOI not more than 10mm; DOI is depth of invasion and not tumor thickness. |
| T3 |
Tumor more than 2 cm and not more than 4 cm with DOI more than 10mm;
or tumor more than 4 cm with DOI not more than 10 mm. DOI is depth of invasion and not tumor thickness. |
| T4 | Moderately advanced or very advanced local disease. |
| T4a |
Moderately advanced local disease.
Tumor more than 4 cm with DOI more than 10 mm or tumor invades adjacent structures only (e.g. through coritical bone of the mandible [lower jawbone] or maxilla [upper jawbone], or involves the maxillary sinus or skin of the face). DOI is depth of invasion and not tumor thickness. |
| T4b |
Very advanced local disease.
Tumor invades masticator space (located on either side of the face around the jawbones), pterygoid plates, or skull base and/or encases the internal carotid artery. |
| Node (N) | |
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis. |
| N1 | Metastasis in a single ipsilateral (on the same side) lymph node, 3 cm or smaller in greatest dimension and ENE*(-). |
| N2 |
Metastasis in a single ipsilateral (on the same side) lymph node, 3 cm or smaller in greatest dimension and ENE*(+);
or larger than 3 cm but not larger than 6 cm in greatest dimension and ENE(-); or metastases in multiple ipsilateral lymph nodes, none larger than 6 cm in greatest dimension and ENE(-); or in bilateral (on both sides) or contralateral (on the opposite side) lymph node(s), none larger than 6 cm in greatest dimension, ENE(-). |
| N2a |
Metastasis in single ipsilateral (on the same side) node 3 cm or smaller in greatest dimension and ENE*(+);
or a single ipsilateral node larger than 3 cm but not larger than 6 cm in greatest dimension and ENE(-). |
| N2b | Metastasis in multiple ipsilateral (on the same side) nodes, none larger than 6 cm in greatest dimension and ENE*(-). |
| N2c | Metastasis in bilateral (on both sides) or contralateral (on the opposite side) lymph node(s), none larger than 6 cm in greatest dimension and ENE*(-). |
| N3 |
Metastasis in a lymph node larger than 6 cm in greatest dimension and ENE*(-);
or metastasis in a single ipsilateral (on the same side) node larger than 3 cm in greatest dimension and ENE(+); or multiple ipsilateral, contralateral (on the opposite side) or bilateral (on both sides) nodes, any with ENE(+); or a single contralateral node of any size and ENE(+). |
| N3a | Metastasis in a lymph node larger than 6 cm in greatest dimension and ENE*(-). |
| N3b |
Metastasis in a single ipsilateral (on the same side) node larger than 3 cm in greatest dimension and ENE*(+);
or multiple ipsilateral, contralateral (on the opposite side) or bilateral (on both sides) nodes, any with ENE(+); or a single contralateral node of any size and ENE(+). |
| Metastasis (M) | |
| M0 | No distant metastasis. |
| M1 | Distant metastasis. |
Staging Oral Cancer
| Stage | T | N | M |
| 0 | Tis | N0 | M0 |
| I | T1 | N0 | M0 |
| II | T2 | N0 | M0 |
| III |
T3
T1, T2, T3 |
N0
N1 |
M0
M0 |
| IVA |
T4a
T1, T2, T3, T4a |
N0, N1
N2 |
M0
M0 |
| IVB |
Any T
T4b |
N3
Any N |
M0
M0 |
| IVC | Any T | Any N | M1 |