Head & Neck
Thyroid Cancer
Includes illustrated staging details
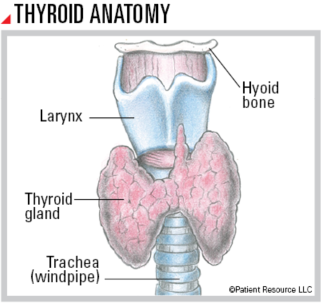
The thyroid gland is located below the larynx (voice box) in the front of the neck. Shaped like a butterfly, it produces hormones that regulate heart rate, body temperature, growth and metabolism. It also contains four parathyroid glands (not shown) that are pea-sized organs on the back of the thyroid. They produce hormones that control blood calcium levels.
Thyroid tissues contain two types of cells. Follicular cells produce the thyroid hormone, and parafollicular cells (commonly called C-cells) produce a hormone involved in processing calcium.
Although thyroid cancer is often not accompanied by many symptoms, it is sometimes discovered on imaging scans or other tests performed to diagnose another medical condition. There are four main types of thyroid cancer: papillary, follicular, medullary and anaplastic.
Of the four, papillary thyroid cancer is the most common. It begins in the follicular cells, as does follicular thyroid cancer. Both are called well-differentiated cancers because their cells look similar to healthy thyroid cells when viewed under a microscope. These typically spread and grow slowly.
Medullary thyroid cancer begins in the C-cells and is more aggressive than papillary or follicular thyroid cancer.
Anaplastic thyroid cancer is called undifferentiated or poorly differentiated because its cells look very different from healthy thyroid cells. It tends to grow and spread very quickly and is the most aggressive form of thyroid cancer.
Treatment Options
Your doctor will develop a treatment plan based on the type and stage of the thyroid cancer as well as your age, overall health, symptoms, previous treatments and preferences for quality of life. One or more of the following therapies may be recommended.
Surgery is the most common treatment for thyroid cancer, and various procedures and techniques may be available. Your surgeon may also remove lymph nodes in the neck to see whether the cancer has spread.
Lobectomy, also called hemithyroidectomy, may be used in some low-risk cases when only half of the thyroid needs to be removed.
Near-total thyroidectomy is used to remove all but a very small part of the thyroid. Some lymph nodes may also be removed.
Total thyroidectomy removes the entire thyroid gland. As a result, thyroid hormone therapy must be taken after surgery because thyroid hormones can no longer be produced in the body.
Radioactive iodine treatment can be used to destroy remaining thyroid cells that were not removed by surgery or that have spread beyond what can be removed with surgery. This involves giving radioactive iodine (I-131) in liquid or pill form. The thyroid absorbs almost all iodine that enters the body. The radioactive iodine will concentrate in any remaining thyroid tissue, and the radiation will kill the cancer cells.
This treatment is standard of care for papillary or follicular thyroid cancer that has spread to lymph nodes in the neck or other parts of the body. Radioactive iodine treatment is not effective in medullary thyroid cancer or anaplastic thyroid cancer because the cancer cells do not absorb iodine.
Radiation therapy is typically given after surgery and concentrates on targeted cancer cells in a specific area. It is more often used as part of treatment for medullary and anaplastic thyroid cancers. External-beam radiation therapy is often used for later stage thyroid cancer that has spread to critical areas of the neck, such as the trachea, voice box or esophagus.
Drug therapy is systemic therapy that travels throughout the body and may include chemotherapy, hormone therapy or targeted therapy.
Chemotherapy uses drugs to destroy cancer cells by preventing them from growing and dividing. It may consist of a single drug or multiple drugs given in combination. It may also be combined with other types of treatment.
Hormone therapy is used after surgery to replace the hormone needed by the body after part of or the whole thyroid is removed. It may also slow the growth of remaining differentiated cancer cells. This medication is a pill. Taking calcium and vitamin D supplements may be necessary if the parathyroid gland function is affected by surgery.
Targeted therapy helps slow or stop the progression of disease in certain types of thyroid cancer. Two types approved for thyroid cancer include tyrosine kinase inhibitors, which block signals needed for tumors to grow, and protein kinase inhibitors, which block proteins needed for cell growth and may kill cancer cells. They may be an option if specific molecular (genetic) abnormalities are found in the tumor. Some of these abnormalities include a neurotrophic tyrosine receptor kinase (NTRK) genetic fusion, a BRAF V600E gene mutation and RET mutation-positive cancers. In some cases, targeted therapy may be used to treat certain types of metastatic thyroid cancer.
Watchful waiting is a strategy to avoid treatment and potential side effects for as long as possible. It may be recommended for tumors that appear to be growing very slowly. Your doctor will closely monitor you for signs the cancer has progressed or returned before starting treatment.
TNM Classification for Thyroid Cancer
| Classification | Definition |
| Tumor (T) | |
| TX | Primary tumor cannot be assessed. |
| Tis | No evidence of primary tumor. |
| Anaplastic & Differentiated | |
| T1 | ≤ (not more than) 2 cm in greatest dimension limited to the thyroid. |
| T1a | ≤ (not more than) 1 cm in greatest dimension limited to the thyroid. |
| T1b | > (more than) 1 cm but ≤ (not more than) 2 cm in greatest dimension limited to the thyroid. |
| T2 | > (more than) than 2 cm but ≤ (not more than) 4 cm in greatest dimension limited to the thyroid. |
| T3 | > (more than) 4 cm limited to the thyroid, or gross extrathyroidal extension (extended beyond the thyroid) invading only strap muscles. |
| T3a | > (more than) 4 cm limited to the thyroid. |
| T3b | Gross extrathyroidal extension (extended beyond the thyroid) invading only strap muscles (sternohyoid, sternothyroid, thyrohyoid or omohyoid muscles) from a tumor of any size. |
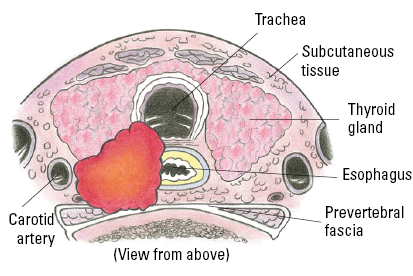
| T4 | Includes gross extrathyroidal extension (extended beyond the thyroid) beyond the strap muscles. |
| T4a | Gross extrathyroidal extension (extended beyond the thyroid) invading subcutaneous soft tissues, larynx, trachea, esophagus, or recurrent laryngeal nerve from a tumor of any size. |
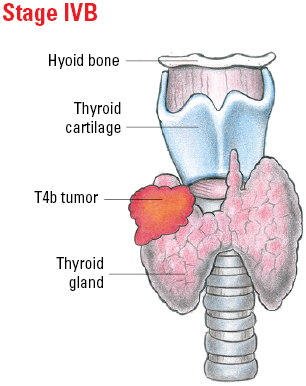
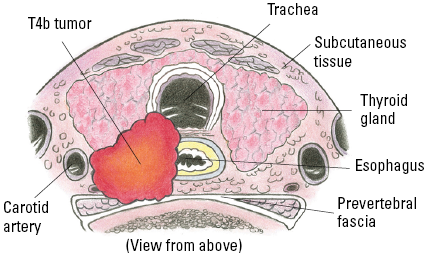
| T4b | Gross extrathyroidal extension (extended beyond the thyroid) invading prevertebral fascia or encasing the carotid artery or mediastinal vessels from a tumor of any size. |
| Medullary | |
| T1 | ≤ (not more than) 2 cm in greatest dimension limited to the thyroid. |
| T1a | ≤ (not more than) 1 cm in greatest dimension limited to the thyroid. |
| T1b | > (more than) 1 cm but ≤ (not more than) 2 cm in greatest dimension limited to the thyroid. |
| T2 | > (more than) 2 cm but ≤ (not more than) 4 cm in greatest dimension limited to the thyroid. |
| T3 | > (more than) 4 cm or with extrathyroidal extension (extended beyond the thyroid). |
| T3a | > (more than) 4 cm in greatest dimension limited to the thyroid. |
| T3b | Tumor of any size with gross extrathyroidal extension (extended beyond the thyroid) invading only strap muscles (sternohyoid, sternothyroid, thyrohyoid or omohyoid muscles). |
| T4 | Advanced disease. |
| T4a | Moderately advanced disease; tumor of any size with gross extrathyroidal extension (extended beyond the thyroid) into the nearby tissues of the neck, including subcutaneous soft tissue, larynx, trachea, esophagus or recurrent laryngeal nerve. |
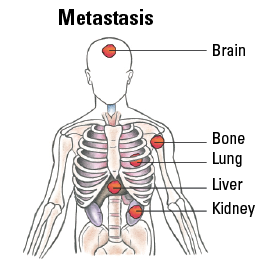
| T4b | Very advanced disease; tumor of any size with extension toward the spine or into nearby large blood vessels, gross extrathyroidal extension (extended beyond the thyroid) invading the prevertebral fascia, or encasing the carotid artery or mediastinal vessels. |
| Node (N) | |
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No evidence of locoregional lymph node metastasis. |
| N0a | One or more cytologically (based on fine needle aspiration biopsy) or histologically (based on pathologic analysis of tissues after surgery) confirmed benign lymph nodes. |
| N0b | No radiologic or clinical evidence of locoregional lymph node metastasis. |
| N1 | Metastasis to regional nodes. |
| N1a | Metastasis to level VI or VII (pretracheal, paratracheal, or prelaryngeal/Delphian, or upper mediastinal) lymph nodes. This can be unilateral (on one side) or bilateral (on both sides) disease. |
| N1b | Metastasis to unilateral (on one side), bilateral (on both sides), or contralateral (opposite side of thyroid tumor) lateral lymph nodes (levels I, II, III, IV or V) or retropharyngeal lymph nodes. |
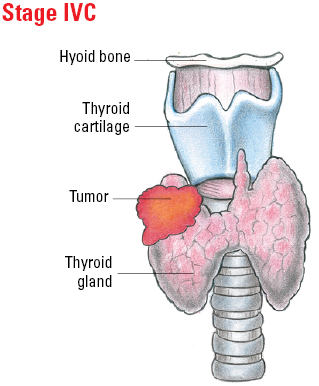
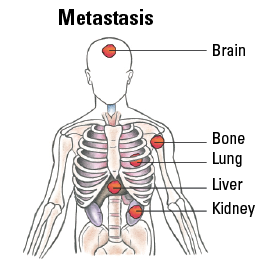
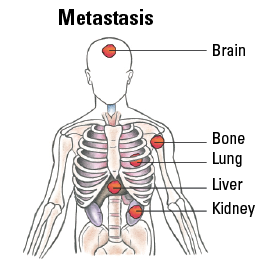
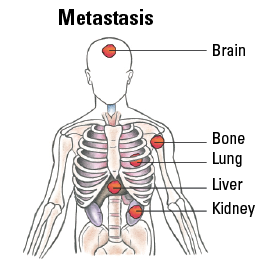
| Metastasis (M) | |
| M0 | No distant metastasis. |
| M1 | Distant metastasis. |
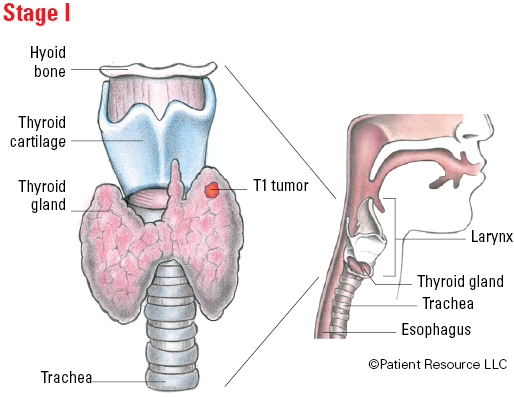
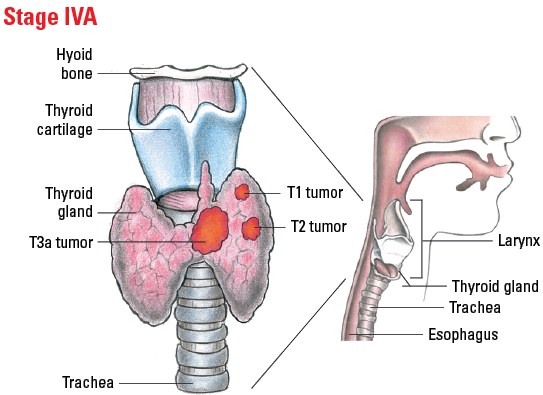
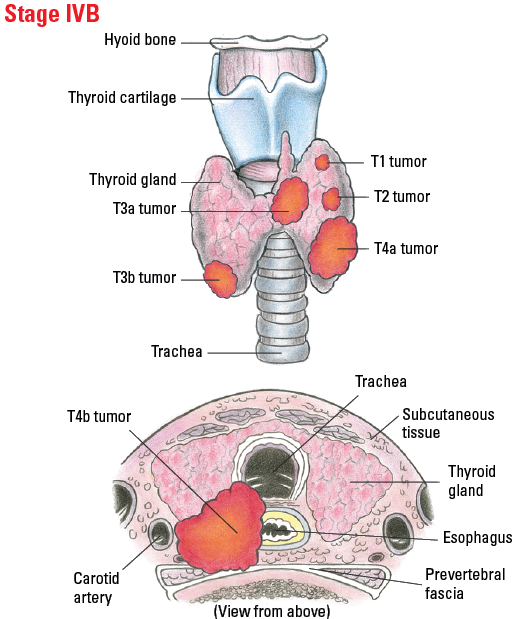
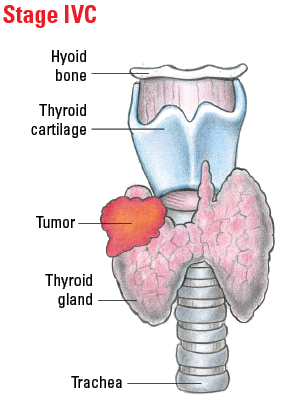
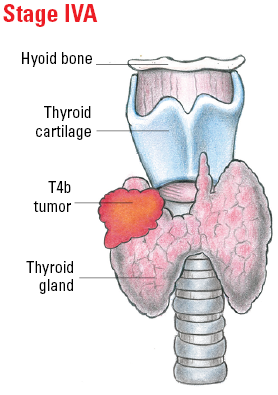
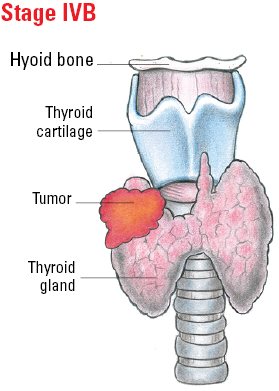
Staging Anaplastic Thyroid Cancer
| Stage | T | N | M |
| IVA | T1-T3a | N0/NX | M0 |
| IVB |
T1-T3a
T3b, T4 |
N1
Any N |
M0
M0 |
| IVC | Any T | Any N | M1 |
Illustrated Stages of Anaplastic Thyroid Cancer
Staging Differentiated Thyroid Cancer
| Stage | T | N | M |
| Younger than 55 years | |||
| I | Any T | Any N | M0 |
| II | Any T | Any N | M1 |
| 55 years or older | |||
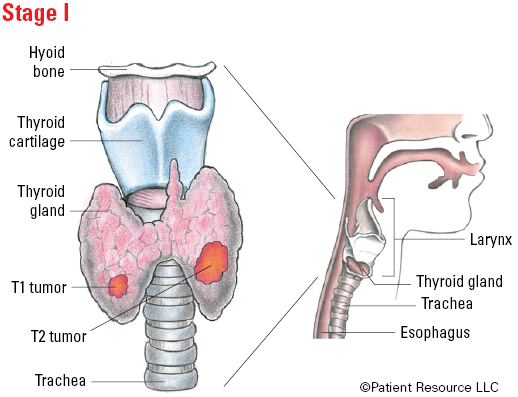
| I | T1, T2 | N0/NX | M0 |
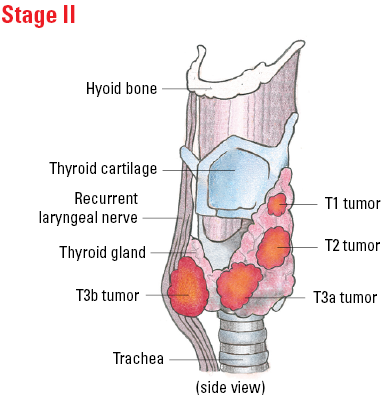
| II |
T1, T2
T3a, T3b |
N1
Any N |
M0
M0 |
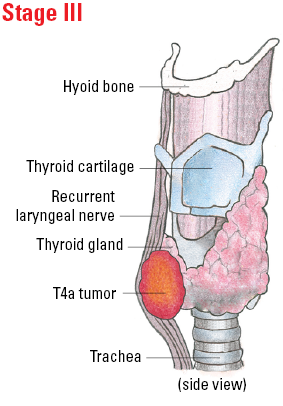
| III | T4a | Any N | M0 |
| IVA | T4b | Any N | M0 |
| IVB | Any T | Any N | M1 |
Illustrated Stages of Differentiated Thyroid Cancer (younger than 55)
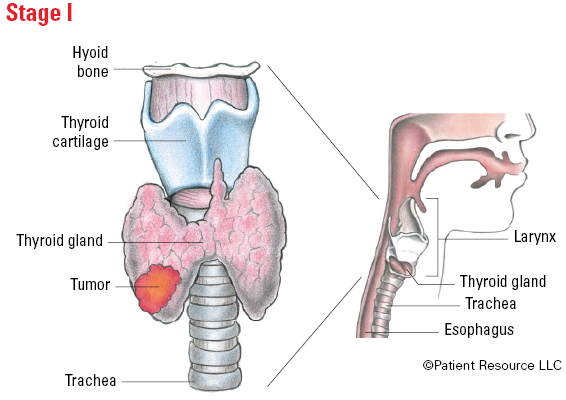
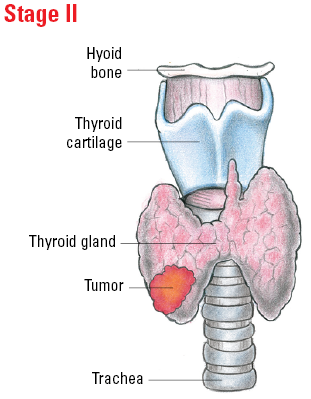
Illustrated Stages of Differentiated Thyroid Cancer (55 and older)
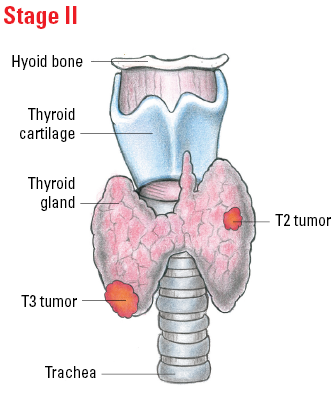
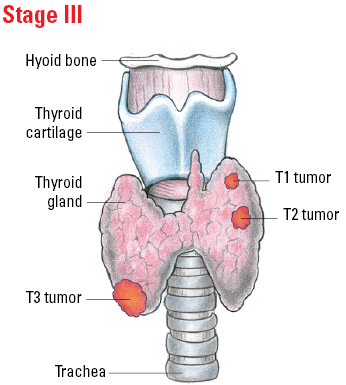
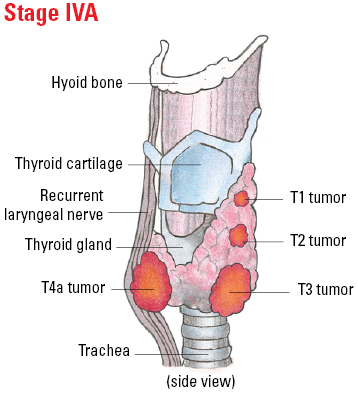
Staging Medullary Thyroid Cancer
| Stage | T | N | M |
| I | T1 | N0 | M0 |
| II | T2, T3 | N0 | M0 |
| III | T1-T3 | N1a | M0 |
| IVA |
T4a
T1-T3 |
Any N
N1b |
M0
M0 |
| IVB | T4b | Any N | M0 |
| IVC | Any T | Any N | M1 |
Illustrated Stages of Medullary Thyroid Cancer