Multiple Myeloma
Introduction
Blood cancers are often difficult to understand because they typically do not include physical tumors, which is what many people think of when they hear the term “cancer.” If you or a loved one has been diagnosed with multiple myeloma, you likely have many questions. Use the following information as a starting point, and talk with your medical team to learn more.
What is multiple myeloma?
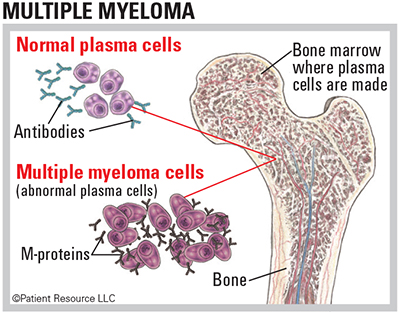
Also referred to as a plasma cell neoplasm, multiple myeloma is a type of hematologic (blood) cancer that begins when the blood’s plasma cells multiply uncontrollably.
Plasma cells are produced in the bone marrow and are a part of the immune system. Healthy plasma cells create antibodies that fight germs and viruses and stop infection. The cells that are multiplying out of control are called myeloma cells.
Healthy cells and myeloma cells both make antibodies, but myeloma cells produce too much of the same antibody. These antibodies are called M-proteins.
The accumulation of myeloma cells usually occurs in multiple areas of bone, giving the disease its name, “multiple myeloma.”
Is there a cure for multiple myeloma?
At this time, a cure for multiple myeloma occurs rarely; however, researchers continue to develop promising treatment strategies, including clinical trials, for managing multiple myeloma as a chronic illness.
What causes multiple myeloma?
The cause of multiple myeloma is unknown. The only two known precursors to multiple myeloma are monoclonal gammopathy of undetermined significance (MGUS) and smoldering myeloma. MGUS occurs when abnormal plasma cells produce too many copies of an identical antibody. Most cases of multiple myeloma are preceded by MGUS, but most patients with MGUS do not develop multiple myeloma. Smoldering myeloma, also called asymptomatic multiple myeloma, is an early stage of myeloma.
How is it diagnosed?
No single symptom or test result will point to multiple myeloma. Instead, it may take many tests to reach a definitive diagnosis, which is why multiple myeloma may be at an advanced stage before you are aware of it.
Your medical team will likely examine the results from blood and urine tests as well as a bone marrow biopsy and imaging tests, including magnetic resonance imaging (MRI) and positron emission tomography combined with computed tomography (PET/CT), and X-rays.
Because researchers have discovered that certain chromosome and molecular abnormalities may be present in multiple myeloma cases, genomic tests may be ordered (see Genomic Testing & Biomarkers).
Your doctor may check for amyloidosis, which is a buildup of amyloid, an abnormal protein. To do so, a biopsy is done on abdominal fat. Differentiating between amyloidosis and multiple myeloma may be part of the diagnostic process.
During the diagnostic process, you may hear the acronym “CRAB.” It stands for the four common signs of multiple myeloma. After the diagnosis process, your doctor will continue to monitor you regularly so any CRAB signs or symptoms can be addressed right away.
How will multiple myeloma affect me on a daily basis?
Some side effects of the illness and its treatment can be noticed by you while others are evident only on test results, making it critical that you stay on schedule with follow-up medical appointments. Some common side effects include the following:
- Weak bones and pain. Myeloma cells collect in solid bone, causing holes called lytic lesions that thin and weaken bones. This can result in pain and, in some cases, fractures. Because the diagnosis process is often lengthy, many people already have lytic lesions by the time they receive their diagnosis.
- Signs of anemia, bleeding, bruising and infection. Myeloma cells can also overcrowd the bone marrow, which suppresses the growth of healthy cells that produce blood. When bone marrow cannot produce enough healthy cells, it can lead to anemia, bleeding and infection. Some signs of anemia include feeling tired, weak, short of breath and dizzy.
- Organ damage. You may have kidney or other organ damage.
What should I do next?
If possible, find a hematologist or oncologist who specializes in diagnosing and treating multiple myeloma. Your doctor or one of the advocacy organizations listed on here can help connect you. Also consider seeking a second opinion as another specialist may be aware of different treatment strategies and clinical trials. Learn about all of your treatment options so you can make the most informed decisions about your care.
CRAB
Calcium level – Elevated calcium levels in the blood
Renal (kidney) function – Kidney damage or failure resulting from the multiple myeloma protein
Anemia – Low red blood cell counts caused by cancer cells slowing the growth of healthy bone marrow cells
Bone lesions – Bone damage (lytic lesions), thinning of the bones (osteoporosis) or a compression fracture of the spine