Pain
Pain medications
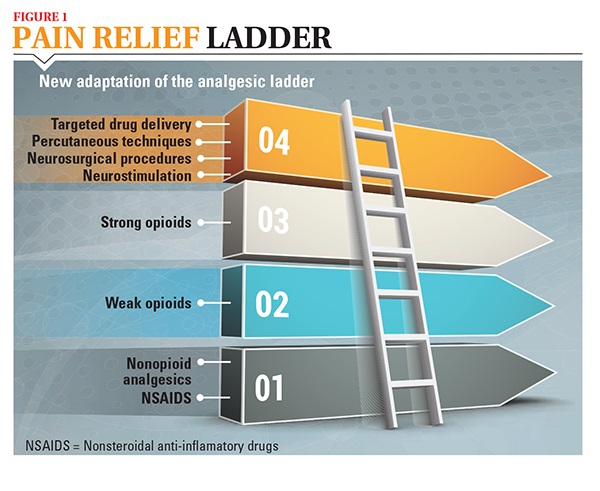
One of the most common ways to alleviate pain is to take over-the-counter and doctor-prescribed medications, a practice known as pharmacotherapy. Oral pain medication is usually the first step in relieving pain, and your doctor will most likely start with weak pain medications and switch to stronger medications if your pain is unrelieved. This stepped process is known as the analgesic ladder (see Figure 1). Your doctor and you will decide how to best manage your pain, using the analgesic ladder as a guide.
Types of pain medications
Mild pain can often be controlled with over-the-counter pain relievers, whereas more severe pain will likely require stronger medications that must be prescribed by your doctor. Newer strong pain medications are now available to be given in a variety of ways and include the following:
- A pill or tablet taken orally (by mouth)
- A pill or spray taken sublingually (under the tongue)
- A tablet held in the buccal mucosa (inside the cheek)
- A cream or spray applied topically (applied to the skin)
- Transdermal (applied to the skin)
The most commonly used medications for pain include:
- Non-steroidal anti-inflammatory drugs (NSAIDs) or Non-opioid analgesics – mostly available over the counter, these medications are intended to relieve mild-to-moderate pain.
- Opioid analgesics or pain relievers –prescribed by doctors to relieve moderate-to-severe pain.
- Adjuvant analgesics – medications designed to provide pain relief, often to treat pain related to damaged nerve cells or nerve swelling, by changing how these nerves generate pain signals.
- Bone-modifying agents – drugs that are taken to help reduce pain related to bone complications from metastatic cancer.
Taking your medication
Pain medication is much more effective when it is taken at regular intervals; a long-acting medication is usually given for this purpose. In this way, you can “stay ahead” of the pain. The most important way you can help ensure the maximal effectiveness of your pain medication is to take your pain medication at the specific intervals your doctor prescribes. Your doctor should also tell you how to manage breakthrough pain (see pyramid below), which is pain that suddenly peaks above baseline pain for a variety of reasons.
You can also help ensure that your pain medication is effective by keeping track of your pain level and how well and for how long your medication is working. For example, tell your doctor if your pain medication is not relieving your pain adequately or if there is a prolonged period of time before pain is relieved. Your doctor may decide that you need a different dose of the pain medication, a different pain medication or a combination of medications, including adjuvant medications.
Some people with cancer-related pain find it helpful to keep a pain diary. With a pain diary, you can keep track of the details of your pain, such as the following:
- Words that describe the pain (aching, burning)
- Name, dose and time you take your pain medication
- Your pain rating (on a scale of zero to ten) at various times during the day, especially after you have taken pain medication
- How long the pain medication works
- When you use other pain-relief methods (such as relaxation techniques, distraction or imagery)
- Side effects you have from the medication
Treating Breakthrough Pain
Breakthrough pain comes on suddenly during regular treatment with pain medications. This can be spontaneous for no apparent reason or provoked by movement or other factors. Be sure to tell your doctor if you have breakthrough pain so that he or she can prescribe specific treatment. Most pain medication is long-acting, but breakthrough pain requires a short-acting drug that works quickly. These drugs are often called "rescue medications." Unlike regular pain medication, medication for breakthrough pain is taken as needed as soon as pain begins; don't try to "wait it out" because it can become worse and more difficult to manage. Be sure to tell your doctor if you have breakthrough pain more than four times a day, if the breakthrough pain is getting worse, or if the breakthrough medication does not relieve the pain.
Safety is key
Most pain medications are very strong, and while taking them to manage cancer-related pain is safe, there are important steps to making sure you, as well as your family and friends, stay safe. When discussing pain medications with your doctor, be sure to tell him or her about other medications you take (including over-the-counter drugs and supplements) and any allergies and other conditions you have (for example, high blood pressure or diabetes). Your doctor needs to know these facts to avoid prescribing a medication that may be harmful to you.
For every prescription medication approved by the FDA, a package insert must accompany the medication. Your doctor, nurse or pharmacist should explain your medications to you and answer any questions you have. Make sure you know the basic information about your medications and how to ensure safety.
Use your pain medications safely
Make sure you know the basic information about your pain medications:
- The dose you should take and when you should take it
- The time it will likely take for the medication to start working
- The length of time relief will last
- Whether to take the medication with food or other medications or supplements
- Other medications that may interact poorly if taken with the medication
- Common and/or potentially serious side effects of the drug
- What to do if you take too much of the medication at one time
- What to do if you miss a dose
- Whether you should keep it refrigerated
Other safety rules for pain medication:
- Do not mix pain medications with alcohol or illicit substances
- Do not share your medication with others
- Keep your medication in a secure location, preferably in a locked box
- Make sure you understand whether you should drive or operate machinery while taking the drug
- Know whom to call if you have questions or concerns
Side effects to expect
Every treatment has possible side effects, but each person’s reaction to a medication is different. Side effects do not occur in every person, and some side effects may be more severe in some people and mild in others. When a pain medication is prescribed for you, ask your doctor, nurse or pharmacist as many questions as needed until you understand the drug you’ll be taking and what the side effects may be.
There are easy ways to manage most of the side effects associated with pain medication. Constipation is one of the most common side effects of opioids. Because of this, most people who are prescribed opioids are encouraged to take a laxative to help alleviate constipation. Nausea, vomiting or confusion may occur in some people when they first start taking a medication, but these side effects usually ease once the person’s body adjusts to the medication. In addition, your doctor can prescribe medications to relieve some side effects.
Open communication
Effectively managing pain relies on open communication between you and your doctor. Some people hesitate to tell their doctor about pain because they don’t want to seem as if they’re complaining. Telling your doctor about pain is not complaining — it is the first step in getting what you need to feel comfortable with a good quality of life.
If you are taking strong pain medications and your pain is still unrelieved or you cannot tolerate the side effects, ask your doctor about seeing a pain specialist who can discuss other options, including interventional approaches.



