Triple Negative Breast Cancer
Treatment Options
New therapies are emerging that are providing a renewed sense of hope to many who have this aggressive disease. Research is ongoing, and the medical community is actively pursuing new forms of treatment for this subset of breast cancer. As a result, you may be a candidate for a clinical trial, which may offer you the chance to have treatments not available to everyone.
Your diagnosis will be factored into your unique treatment plan. Your doctor will consider your age, general health, menopausal status and size and stage of the tumor, as well as biomarkers and genetic testing results. Your plan may include some of the following.
Surgery is often the first option used to treat TNBC and includes either a lumpectomy or a mastectomy. Surgery for TNBC often follows chemotherapy (which is called neoadjuvant chemotherapy). As you consider your surgical options, be aware of the common misperception that surgery eliminates the chance of recurrence.
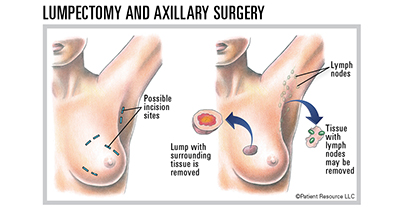
A lumpectomy, also referred to as breast conserving or breast-sparing surgery, removes only the tumor (lump) and a small margin of normal-appearing tissue around the lump (see below). A lumpectomy can be done for most small tumors. It is usually followed by radiation therapy designed to kill microscopic cancer cells hiding in other parts of the breast. For patients with TNBC, chemotherapy is either given before surgery or given after surgery but before radiation.
A mastectomy involves removing the entire breast and may be preferred for larger tumors, especially when they occur in a smaller breast (see below). Several types of mastectomy exist, including total mastectomy and modified radical mastectomy. Total mastectomy surgically removes the entire breast without removing muscle. A modified radical mastectomy is a total mastectomy that is performed along with removing a block of underarm/axillary lymph node tissue (axillary dissection). Your doctor may recommend a mastectomy if you have a large tumor, multiple tumors in the breast or cancer that has spread to the skin, or if you were previously treated with lumpectomy and radiation therapy for a cancer in that same breast.
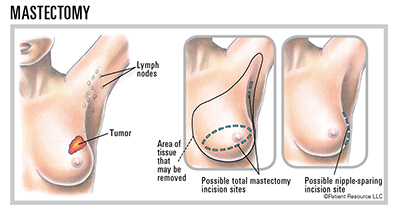
Patients with hereditary breast cancer, such as those with BRCA mutations (see Genetic Testing), may opt to undergo bilateral mastectomy even if they only have a single small tumor as a strategy for reducing their chances of developing a future second breast cancer. Since outcome from breast cancer tends to be determined by the aggressiveness and metastatic risk of a woman’s first breast cancer (rather than whether she chooses mastectomy versus lumpectomy), patients with BRCA mutations may still be candidates for breast-conserving surgery.
Most TNBC, as well as non-TNBC, patients will need to undergo surgery to remove some of the lymph nodes (glands) in the underarm (axillary) region. Information regarding whether or not the breast cancer has spread into these lymph nodes is important prognostically and can influence other aspects of treatment, such as your chemotherapy and radiation plan.
Some patients will be candidates for a relatively small axillary procedure called a sentinel lymph node biopsy, which involves removing only the few most important axillary nodes. Other patients require a more extensive operation to control their disease called an axillary lymph node dissection (see above). The axillary surgery plan that is most appropriate for your cancer will be based upon the extent of your disease and your other treatments, including radiation therapy and chemotherapy.
Additional surgical procedures may be an option for people who have BRCA mutations and/or hereditary breast cancer. These women have a higher-than-average risk for developing new cancers in the contralateral (opposite) breast, or in either breast if they have had a lumpectomy.
Prophylactic mastectomy reduces the risk of a new breast cancer but it does not completely eliminate the risk because microscopic amounts of breast tissue can remain hidden in the skin flaps or in the underarm fatty tissue after a mastectomy. Talk to your doctor about these potential options before deciding if prophylactic surgery is right for you.
Radiation therapy uses high-energy X-rays to kill cancer cells or keep them from growing. The most common type of radiation is external-beam radiation therapy (EBRT).
Radiation therapy is almost always delivered after lumpectomy to destroy any cancer cells that may be hidden in normal-appearing breast tissue. Post-mastectomy radiation therapy is sometimes necessary, particularly for people who face a high risk of the cancer growing back on the chest wall area (mastectomy skin flaps, underarm/axillary region). Post-mastectomy radiation therapy can lower this risk.
Chemotherapy uses powerful drugs to kill rapidly multiplying cells throughout the body. Neoadjuvant (preoperative) chemotherapy is used frequently with TNBC to shrink a large, bulky tumor so it can be removed surgically or to reduce the tumor’s size so a patient can undergo a lumpectomy rather than a mastectomy. Neoadjuvant chemotherapy also helps the doctor determine how well the chemotherapy drugs work against the tumor.
Adjuvant chemotherapy is given postoperatively to destroy cancer cells that may remain, some of which may be too small to detect with laboratory testing or imaging studies. This can be lifesaving and decrease the risk of recurrence in higher-risk patients and most patients with TNBC.
Targeted therapy uses drugs or other substances to attack specific types of cells that play important roles in the growth and survival of cancer cells.
It is used to treat breast cancer in patients with BRCA mutations. A poly (ADP ribose) polymerase (PARP) inhibitor targets HER2-negative cancers associated with a BRCA1 or BRCA2 mutation. PARPs are a family of enzymes that are involved with a DNA repair gene, which is often present in TNBC.
Immunotherapy uses the body’s own immune system to recognize and attack cancer cells that have been hiding and targets them for destruction. Immune checkpoint inhibitors target the protein PD-L1 (programmed death-ligand 1) found on cells and boost the immune system’s cancer-fighting response.
In some cases, patients may qualify for tumor-agnostic treatment. This is a new class of drug therapy that is approved to treat solid tumors anywhere in the body that meet specific criteria:
- It is only available for people with tumors that are metastatic or unresectable (cannot be removed with surgery).
- The tumor must contain a greater than normal amount of molecular alterations.
- The cells must contain a mutation that prevents them from fixing errors that occur during duplication.
| Commonly Used Medications |
|
CHEMOTHERAPY
Combinations
|
|
TARGETED THERAPY
PARP inhibitors
|
As of 10/8/19
Breast reconstruction may be an option to consider after having a lumpectomy or mastectomy. Breast reconstructive surgery, which should be performed by an experienced plastic surgeon, is typically started or even completed at the same time as a mastectomy but can happen later (within months or even years after the mastectomy, depending on individual circumstances). It may be done during or after a lumpectomy when the surgery will cause the affected breast to appear significantly different from the other.
Different breast reconstruction techniques are available. They may involve the use of a breast implant or a flap of tissue (usually containing skin, fat, possibly muscle and blood vessels) from elsewhere in your body, or a combination of the two. The use of a tissue flap depends on the size of your breasts, your body type and preferences regarding appearance.
Reconstructive Techniques
With an Implant A breast implant filled with silicone gel or saline (salt water) may sometimes be placed following the mastectomy in a single operation referred to as immediate reconstruction. In delayed reconstruction, a tissue expander is inserted under the skin following the mastectomy to gradually stretch the skin and underlying tissue; an implant is then placed in a second surgery, often when treatment is completed.
With a Tissue "FLAP" A tissue “flap” usually contains skin, fat, blood vessels and sometimes muscle. A pedicle flap remains attached to the body and is repositioned to the breast area with a muscle carrying the blood supply. A free flap is removed from the body along with blood vessels, which are then attached to the blood vessels in the breast area. Some types of flaps follow.
[DIEP] deep inferior epigastric perforator flap
[SIEA] superficial inferior epigastric artery flap
[TRAM] transverse rectus abdominis muscle flap
[LD] latissimus dorsi flap
[GAP] gluteal artery perforator flap (gluteal free flap)
[SGAP] superior gluteal artery perforator flap
[PAP] profunda artery perforator flap
[TUG] transverse upper gracilis flap
Reconstruction requires a long healing period, which could delay the start of chemotherapy or interfere with potential radiation therapy. If you’re considering reconstructive surgery (even if it will be done later), discuss this with your cancer surgeon and a plastic surgeon before the mastectomy so they can properly plan your treatment.
Non-surgical options to restore the breast appearance also exist. If you prefer not to have additional surgery but want the appearance of breasts or while you are waiting to have reconstructive surgery later, you may consider a breast prosthesis. Or, you may choose none of these options, also referred to as “going flat.” Talk with your doctor about the options that are available to you.
If Breast Cancer Returns
Cancer recurrence is when the breast cancer comes back in the chest wall or in the same or opposite breast or in a distant site after initial treatment. Recurrent breast cancer may occur months or years after initial treatment. The cancer may come back in the same place as the original cancer (local recurrence), or it may spread to other areas of your body. If it recurs in the lymph nodes on the same side as the original breast cancer, it is called a regional recurrence. Local and regional recurrences usually occur on the same side of the body as the original breast cancer; the development of cancer in the contralateral (opposite) breast typically represents a completely new breast cancer. When breast cancer recurs in a different organ of the body (such as the liver, lungs or bones), this is called distant, or metastatic, recurrence. All metastatic recurrences are considered advanced disease.



