Melanoma
Staging Becomes the Foundation of Your Treatment Plan
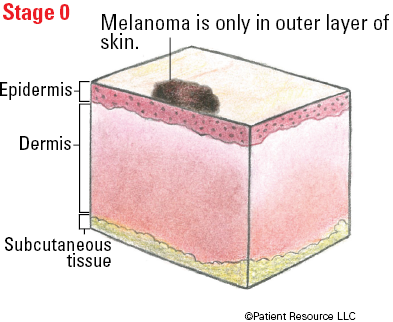
Once your diagnosis is made, a process called staging is used to determine the extent of the cancer within your body. This section is designed to help you better understand how staging enables your doctor to select the treatment options that will be most effective for you.
Melanoma is usually staged twice. First, your doctor considers the results of your physical exam and skin biopsy to assign a clinical stage. During a more extensive procedure, the lesion (or as much of it as possible) is removed along with some healthy tissue surrounding it. In a different procedure, some lymph nodes may be removed. After reviewing these specimens with and without a microscope and noting key characteristics, a pathologist also considers results from lymph node biopsies and other tissue that was examined. Then a pathologic stage is assigned. Because the pathologic stage is based on more details about the melanoma, this staging is the most accurate and is important in determining the best treatment options for your diagnosis.
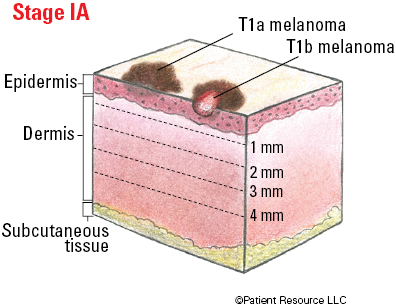
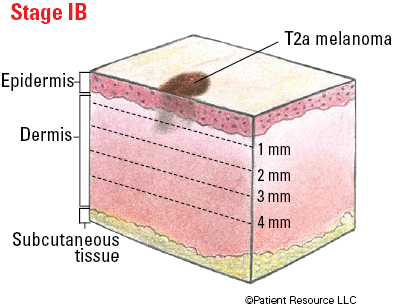
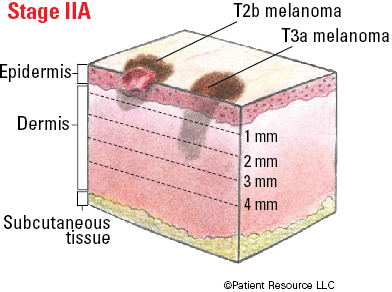
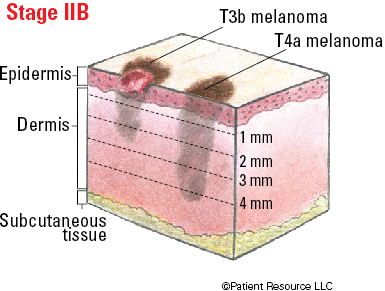
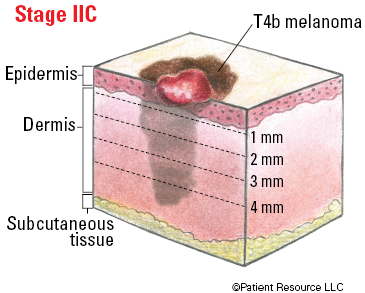
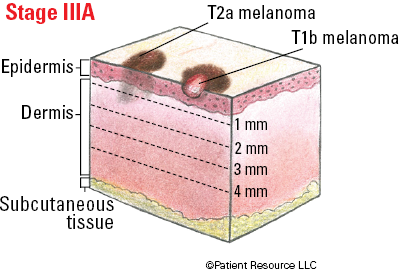
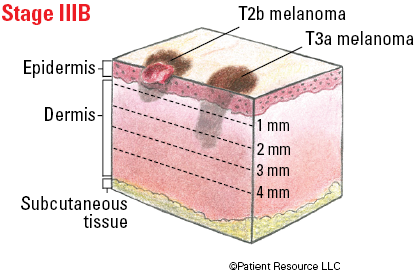
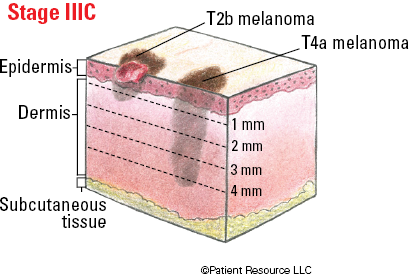
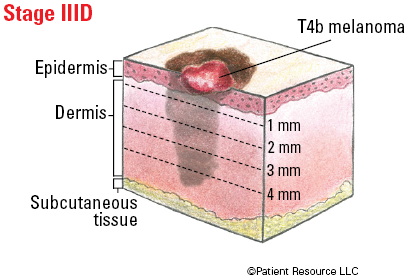
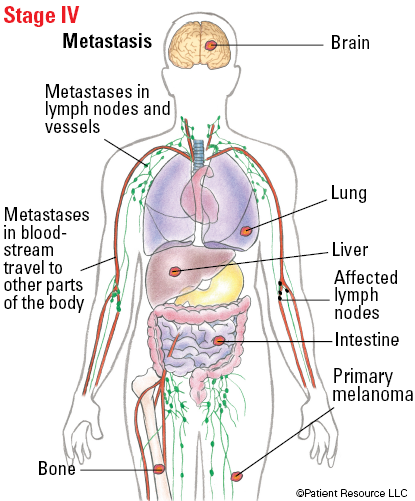
Both the clinical and pathologic stages of melanoma are classified according to the tumor, node, metastasis (TNM) system developed by the American Joint Committee on Cancer (AJCC). This system uses the size and location of the tumor (T), whether cancer cells are found in nearby lymph nodes (N) and whether the cancer has metastasized, or spread, to other parts of the body (M). The thickness of the primary melanoma is used to classify the melanoma in the T category. Additionally, each T classification is further divided into groups according to whether ulceration (a break in the outer layer of skin over the melanoma) is absent (subcategory a) or present (subcategory b). The node (N) classification is used to describe how many lymph nodes contain melanoma cells and includes subcategories to describe the extent of cancer cells in the lymph nodes.
The results of the TNM analysis are then used to determine the overall stage of melanoma for each individual. Stages range from 0 to IV (see Tables 1 and 2).
Table 1 - AJCC TNM System for Classifying Melanoma of the skin
| Classification | Definition | |
| Tumor (T) | ||
| T Category | Thickness | Ulceration Status |
| TX | Primary tumor cannot be assessed | Not applicable |
| T0 | There is no evidence of primary tumor | Not applicable |
| Tis | Melanoma in situ | Not applicable |
| T1 | ≤ (not more than) 1.0 mm. | Unknown or unspecified |
| T1a | < (less than) 0.8 mm. | Without ulceration |
| T1b |
< (less than) 0.8 mm.
< 0.8 – 1.0 mm. |
With ulceration
With or without ulceration |
| T2 | > (more than) 1.0 – 2.0 mm. | Unknown or unspecified |
| T2a | > (more than) 1.0 – 2.0 mm. | Without ulceration |
| T2b | > (more than) 1.0 – 2.0 mm. | With ulceration |
| T3 | > (more than) 2.0 – 4.0 mm. | Unknown or unspecified |
| T3a | > (more than) 2.0 – 4.0 mm. | Without ulceration |
| T3b | > (more than) 2.0 – 4.0 mm. | With ulceration |
| T4 | > (more than) 4.0 mm. | Unknown or unspecified |
| T4a | > (more than) 4.0 mm. | Without ulceration |
| T4b | > (more than) 4.0 mm. | With ulceration |
| Node (N) | ||
| N Category | Number of tumor-involved regional lymph nodes | Metastases status* |
| NX | Regional nodes not assessed. | No |
| N0 | No regional metastases detected. | No |
| N1 | One tumor-involved node or in-transit, satellite, and/or microsatellite metastases with no tumor-involved nodes. | |
| N1a | One clinically occult. | No |
| N1b | One clinically detected. | No |
| N1c | No regional lymph node disease. | Yes |
| N2 | Two or three tumor-involved nodes or in-transit, satellite, and/or microsatellite metastases with one tumor-involved node. | |
| N2a | Two or three clinically occult. | No |
| N2b | Two or three, at least one of which was clinically detected. | No |
| N2c | One clinically occult or clinically detected. | Yes |
| N3 | Four or more tumor-involved nodes or in-transit, satellite, and/or microsatellite metastases with two or more tumor-involved nodes, or any number of matted nodes without or with in-transit, satellite, and/or microsatellite metastases. | |
| N3a | Four or more clinically occult. | No |
| N3b | Four or more, at least one of which was clinically detected, or presence of any number of matted nodes. | No |
| N3c | Two or more clinically occult or clinically detected and/or presence of any number of matted nodes. | Yes |
| * In-transit metastases occur more than 2 cm from the primary melanoma (both on the surface of the skin or below the surface of the skin) to the regional lymph nodes. Satellite metastases occur on or below the skin within 2 cm of the primary melanoma. Microsatellite metastases in the skin or in the deeper layer of the dermis near or deep within the skin of the primary melanoma is detected upon microscopic examination. | ||
| Metastasis (M) | ||
| M Category* | Anatomic site | LDH level |
| M0 | No evidence of distant metastasis. | Not applicable |
| M1 | Evidence of distant metastasis. | See below |
| M1a | Distant metastasis to skin, soft tissue including muscle, and/or nonregional lymph node. | Not recorded or unspecified |
| M1a(0) | Not elevated | |
| M1a(1) | Elevated | |
| M1b | Distant metastasis to lung with or without M1a sites of disease. | Not recorded or unspecified |
| M1b(0) | Not elevated | |
| M1b(1) | Elevated | |
| M1c | Distant metastasis to non-CNS visceral sites with or without M1a or M1b sites of disease. | Not recorded or unspecified |
| M1c(0) | Not elevated | |
| M1c(1) | Elevated | |
| M1d | Distant metastasis to CNS with or without M1a, M1b, or M1c sites of disease. | Not recorded or unspecified |
| M1d(0) | Normal | |
| M1d(1) | Elevated | |
| *Suffixes for M category: (0) LDH not elevated, (1) LDH elevated. No suffix is used if LDH is not recorded or is unspecified. | ||
Table 2 - Stages of Melanoma of the Skin
| Stage | T | N | M |
| 0 | Tis | N0 | M0 |
| IA |
T1a
T1b |
N0
N0 |
M0
M0 |
| IB | T2a | N0 | M0 |
| IIA |
T2b
T3a |
N0
N0 |
M0
M0 |
| IIB |
T3b
T4a |
N0
N0 |
M0
M0 |
| IIC | T4b | N0 | M0 |
| IIIA | T1a/b-T2a | N1a or N2a | M0 |
| IIIB |
T0
T1a/b-T2a T2b/T3a |
N1b, N1c
N1b/c or N2b N1a-N2b |
M0
M0 M0 |
| IIIC |
T0
T1a-T3a T2b/T4a T4b |
N2b, N2c, N3b or N3c
N2c or N3a/b/c Any N ≥ N1 N1a-N2c |
M0
M0 M0 M0 |
| IIID | Any T, Tis | Any N | M0 |
| IV | Any T, Tis | Any N | M1 |
More About Your Pathology Report
With today’s emphasis on personalizing treatment for each person’s cancer, including its genomic or molecular abnormalities, pathology report results are integral to melanoma treatment. Doctors have more options for treating melanoma by subtype now that drug therapies are available for targeting specific mutations, but these therapies can only be used if they are confirmed with genomic or molecular testing.
Along with your diagnosis and histologic subtype (classification based on the melanoma’s microscopic features), your pathology report may include some or all of the following:
Thickness: how deep the tumor has grown into the skin
Ulceration status: whether the tumor’s top skin layer is present and intact (not ulcerated) or broken or missing (ulcerated)
Dermal mitotic rate: how many melanoma cells are actively growing and dividing
Peripheral margin status: the presence or absence of cancer cells in the normal-looking tissue that was removed from around the tumor
Deep margin status: the presence or absence of cancer cells in the normal-looking tissue that was removed from underneath the tumor
Microsatellitosis: the presence of tiny satellite tumors that have spread to skin near the first melanoma tumor. These can only be seen with a microscope.
Regression: the presence of lymphocytes (a type of white blood cell) and scar-like changes that suggest a person’s immune system is attacking the melanoma
Location: where the tumor is found
Tumor-infiltrating lymphocytes: the presence of white blood cells that may be present in a primary melanoma
Vertical growth phase: evidence of tumor growth down into the skin
Angiolymphatic invasion: whether melanoma has grown into blood or lymph vessels
Neurotropism: the presence of melanoma cells in or around the nerves in the skin
Ask your doctor to explain how these findings affect your treatment options. You can also request a copy of your pathology report.
Illustrated Stages of Melanoma of the Skin