Breast Cancer
Overview
Even though breast cancer may be the most common type of cancer diagnosed today, your diagnosis is as unique as you are. Know that there are things you can do to prepare for the path ahead.
First, find a skilled medical team that has experience treating your type of breast cancer. The relationship you have with your doctor, nurse navigator and other members of the team will last for some time, and feeling comfortable with them is essential. You’ll be partners, so being confident in their abilities and trusting their recommendations is important. In turn, it’s equally important for you to feel valued and respected. After all, being diagnosed with breast cancer is a highly intimate experience. You’ll share delicate information with the team members and ask for their help as you move forward with your treatment.
Next, adopt the mindset that knowledge is power, and learn as much as you can about your particular type, subtype and stage of breast cancer to determine your goals of treatment. Surgical oncologist Charles M. Balch, MD, FACS, is passionate about ensuring patients are informed. He feels an educated patient is more likely to get better care and is always better equipped emotionally to cope.
“As physicians, when we talk with our patients and their families, we want them to feel they are active participants in their own care. We don’t want to simply tell them how we plan to treat their disease. Instead, we talk about our shared treatment goals and their expectations for their own quality of life. The more they understand, the more comfortable they are making decisions and following their personalized treatment plan.”
Understanding the basics of cancer may help you process your diagnosis. Cells typically divide in an orderly fashion. When worn out or damaged, they die, and new cells replace them. Cancer develops when genes begin to change, or mutate, within the structure of normal cells. These cells – now called cancer cells – grow and push against normal cells.
About Breast Cancer
Breast cancer develops when genes in normal cells mutate and cause the cells to multiply uncontrollably. They form a disorganized mass of billions of abnormal cells called a tumor. It is important to know that breast cancer is not always felt as a lump. Sometimes it is detected as a bloody nipple discharge or on a mammogram or breast ultrasound.
Cancer cells can penetrate and damage nearby organs and tissues. They can also break away from a tumor and spread to other parts of the body through the bloodstream or lymphatic system, a process known as metastasis. However, when breast cancer spreads, such as to the lung, it is still considered breast cancer and treated as such. It does not become lung cancer.
A breast tumor can occur in men as well as women. It is uncommon in men but can develop at any age, with the average age of diagnosis between 65 and 70. Though a lump may seem easy to feel because men typically have less breast tissue, they often ignore it or do not report it to their doctor because they may not realize they are at risk. They also do not obtain screening mammograms. As a result, their diagnoses are often late stage.
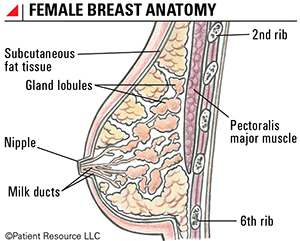
The breasts are made up of connective tissue, fat and glandular tissue that contains the cells that can make milk. Glandular tissue includes the milk ducts, which are thin tubes that carry milk from the lobules to the nipple, and lobules, which are composed of the cells that make milk.
Multiple types of breast cancer exist, but it is important to categorize the cancer as being noninvasive versus invasive at the time of diagnosis. The distinction between these two patterns is confirmed by the microscopic analysis of breast biopsy tissue. Noninvasive breast cancer lacks the ability to spread beyond the ductal or lobular walls. Invasive breast cancer spreads beyond the ductal or lobular structures into surrounding fatty and fibrous breast tissue and other organs. Ductal carcinoma in situ (DCIS) is the most common type of noninvasive breast cancer. Most DCIS cases require therapy (surgery and possibly radiation therapy) to remove and/or treat the abnormal breast tissue and to prevent the development of invasive cancer. Ongoing studies are examining less invasive ways to treat DCIS.
Types of Breast Cancer
| Type | Characteristics | |
| Non-invasive | ||
| Ductal carcinoma in situ (DCIS) | Cancer cells remain confined to the milk ductal units. | |
| Paget disease | Begins in the ducts of the nipple; can be in situ or invasive. | |
| Invasive | ||
| Cribriform | Cancer in connective tissue featuring "holes" within the histologic pattern. | |
| Ductal | Cancer cells that arise from the milk ducts and spread beyond ductal walls into surrounding fatty tissue, connective tissue, lymphatics and/or vascular structures within the breast. | |
| Inflammatory Breast Cancer (IBC) | Cancer that is always staged as either Stage III or Stage IV disease, associated with redness and swelling of the breast. Breast skin may look pitted, resembling an orange peel. IBC may be difficult to diagnose because people often report atypical symptoms. IBC may not form lumps like other breast cancers or show up on a mammogram. Often misdiagnosed as mastitis(an infection of breast tissue). | |
| Lobular | Cancer cells that arise from the lobules (milk-producing glands) and spread into surrounding fatty tissue, connective tissue, lymphatics and/or vascular structures within the breast. | |
| Medullary | Soft, fleshy tumor, often associated with inflammatory cells called lymphocytes; usually has a better prognosis (outlook) than invasive ductal or invasive lobular cancers of the same size. | |
| Metaplastic | Rapidly growing tumor, contains a mixture of cell types, including epithelial (glandular) cells and mesenchymal (bone, skin and muscular) cells. | |
| Mucinous (colloid) | Mucus is primary component of the tumor; less likely to spread to lymph nodes. | |
| Papillary | Tumor with small, finger-like projections; often occurs with DCIS. | |
| Tubular | Typically low grade, ER+, less likely to spread beyond breast. | |
| Receptor subtypes | ||
| Hormone receptor (ER+ and/or PR+) | Tumor positive for estrogen and/or progesterone. | |
| HER2-positive (HER2+) | Tumor overexpresses the HER2 oncogene, includes any ER or PR status. | |
| Triple-negative (ER-/PR-/HER2-) | Tumor negative for ER and PR and does not overexpress HER2. Triple negative breast cancer (TNBC) tends to be more aggressive and is more likely to have microscopic cancer cells hiding in other organs (micrometatstases). Treatment options are limited because therapies that target ER, PR and HER2 will not be effective; however, recent FDA drug approvals offer more treatment options. | |
Getting a Second Opinion
Gathering as much information as you can before starting treatment may help you feel more confident in making the decisions ahead. This may include getting a second or third opinion to confirm the diagnosis and potential treatment options. Another doctor’s opinion may change the diagnosis or reveal a treatment your first doctor was not aware of. And, this is the perfect time to seek out a doctor that specializes in your type of breast cancer who may have access to leading-edge therapies.
Doctors bring different training and experience to treatment planning. Some doctors may favor one treatment approach, while others might suggest a different combination of treatments.
A second opinion is also a way to make sure your pathology diagnosis and staging are accurate, and that you are aware of clinical trials that you might want to consider. You need to hear all the facts about your treatment options. There is often collective wisdom gained from the experience and opinions of different oncology specialists who are experts in your type of cancer.
The process involves asking another cancer specialist or group of specialists to review your medical records and confirm your doctor’s diagnosis and treatment plan. Finding these experts is not always easy, and you may worry that you will offend or hurt your doctor’s feelings if you seek the advice of another expert. Many people feel uncomfortable and even disloyal seeking another opinion, but you should not. Most doctors welcome a second opinion and will recommend another physician or hospital. Above all, the goal is for you to have the best care available.
Before meeting with another medical professional for a second opinion, make sure medical records related to your cancer are available. This may include laboratory, biopsy or imaging test results as well as any other tests or procedures. It may be helpful to call the doctor’s office to find out whether any information needs to be sent ahead of the appointment.
Choosing a Treatment Center
Where to go for your cancer treatment is an important decision, and it may be one you didn’t even realize you could make. This is your cancer diagnosis, and you are in charge. You can ask for help from trusted health care professionals and your loved ones but, ultimately, where you are treated is your decision. Learn what to look for in a treatment facility and discover why it is important to find the right one for you.
Not all treatment centers offer the same features, so start by understanding your breast cancer diagnosis, thinking about your goals of treatment and educating yourself about the services that are available.
Following are some of the services to consider. And, as you interview treatment centers, ask about the other features that are available.
Accreditations. A health care organization that is accredited has demonstrated its ability to meet certain regulatory requirements and standards, which translates to a commitment of providing the highest level of care.
- National Cancer Institute (NCI)-designated cancer centers are recognized for their scientific excellence and extensive resources focused on cancer and cancer-related problems.
- The National Accreditation Program for Breast Centers (NAPBC) is a consortium of national professional organizations focused on breast health and the improvement of quality outcomes.
Clinical trials. Access to available clinical trials for your type of breast cancer may offer a valuable treatment option, especially if you have a rare type of breast cancer or the treatments you have tried are no longer effective.
Breast cancer specialists. Doctors who specialize in your type of breast cancer have more experience, which leads to expertise. Finding a specialist can start with your diagnosing physician. Your family and friends, insurance provider and local and national advocacy groups may also help.
Commitment to technology. Some facilities may be leaders in technological advances for your type of breast cancer, such as newer radiation therapy equipment that targets a tumor with pinpoint accuracy, minimizing damage to surrounding tissues.
Financial considerations. Ask if the facility accepts your insurance plan and whether a financial counselor on staff could refer you to financial assistance resources.
Location. You may prefer to be treated close to home for many reasons, such as convenience, staying near your family, being able to continue to work or cost.
Multidisciplinary care. Certain facilities use the team approach to care and take into account the physical, emotional and psychological effects of a cancer diagnosis. The team may include medical, radiation and surgical oncologists; a diagnostic radiologist; a pathologist; an oncology nurse; a nurse navigator; a pharmacist; an oncology social worker; a dietitian; and/or a chaplain.
Patient navigators. “Patient navigation” refers to the assistance some facilities offer to help patients chart a course through the health care system as well as overcome any barriers to quality care. Patient navigators help patients learn about treatment options, set up appointments with a caregiver, arrange for a translator when needed, coordinate transportation to and from care, secure child care during treatment, arrange financial support for the patient and link patients with follow-up services post-treatment.