Understanding the Genomics and Genetics of Cancer
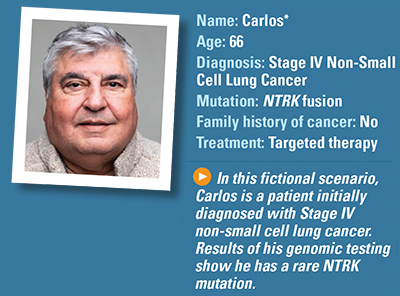
Fictional Case Study: Lung Cancer
What are Carlos’ initial symptoms?
When Carlos experiences shortness of breath and begins coughing, he makes an appointment at an urgent care clinic. He shares his symptoms with the doctor, who performs a physical examination. He listens to his lungs and then orders an X-ray. Results show a mass in the upper right lobe of his lung. The doctor refers him to a local oncologist for further testing.
How is his cancer diagnosed?
The oncologist orders a CT, which shows a right upper lung mass and enlarged hilar and mediastinal lymph nodes, so the oncologist orders a CT-guided biopsy. The tissue specimen is examined by a pathologist, who confirms that the mass is an adenocarcinoma of the lung, which is the most common form of non-small cell lung cancer.
His oncologist also orders a contrast-enhanced MRI of his brain to check for any metastases (spread) of the cancer. The MRI shows one small metastatic lesion of less than 1 centimeter in his brain. Carlos is diagnosed with Stage IV adenocarcinoma of the lung (non-small cell lung cancer).
What additional testing is needed?
The oncologist explains that although initial testing indicates lung cancer, she will request genomic profiling on both a blood sample and on the tissue biopsy to find out whether his cancer has any mutations. She explains that the blood testing will provide results several weeks before the tissue testing. She also explains that a positive result will lead to a specific therapy in the shortest time frame. However, the tissue testing is more sensitive as there is more DNA. Thus, if the blood test is negative, they will await the tissue test results before selecting therapy.
She tells Carlos she’s ordering next-generation sequencing of his samples because many different mutations have been discovered in lung cancer, and this type of test looks for more than one mutation. The testing looks for mutations in the following genes: ALK, BRAF, EGFR, HER2, KRAS, MET, NTRK, RET, ROS1 and STK11. She also includes testing for levels of PD-L1, PD1 and tumor mutational burden (TMB).
If he has a mutation that has approved treatments available, Carlos may have more treatment options, such as an oral targeted therapy pill or an immunotherapy, which may have fewer side effects than traditional chemotherapy. Carlos likes this idea.
He is nervous about waiting, but she assures him that, in his case, delaying the start of treatment for two to three weeks is not likely to affect the outcome.
What are the results of his genomic testing?
Results of the comprehensive biomarker testing show that Carlos has an NTRK fusion, which is fairly rare in non-small cell lung cancer. His oncologist explains that fewer than two percent of non-small cell lung cancers contain the NTRK fusion.
Carlos is concerned that this biomarker is too rare to have a targeted or molecular therapy available, but his doctor assures him that there are some molecular therapies that target the NTRK mutation.
What are his treatment options?
His oncologist explains that she thinks the best course of treatment is to prescribe a molecular therapy known as a tropomyosin receptor kinase (TRK) inhibitor, which is an oral pill, even though he has one lesion in his brain.
She also believes the molecular therapy will help control the brain metastasis because he does not have severe symptoms, and the pill can cross the blood-brain barrier and treat the brain metastasis as well as the lung mass and lymph node metastases.
How does Carlos do on treatment?
Carlos tolerates the drug well and has few side effects. He is grateful he did not have to have chemotherapy and that he is not losing his hair.
Follow-up testing shows the cancer responds well to the treatment. However, Carlos begins having trouble breathing again after nine months of treatment. His oncologist orders a repeat chest CT scan and discovers that the tumor in his lung is back. She suspects the cancer has developed resistance to the TRK inhibitor and appears to be no longer working to control the cancer.
What treatment options are available now?
The oncologist explains that it is common for cancer to develop resistance to a TRK inhibitor, and she reassures him that other options are available. She explains that the first drug he took was considered a first-generation TRK inhibitor and they can try a newer second-generation TRK inhibitor. That is the therapy she prescribes.
How does Carlos respond to the new inhibitor?
He tolerates the new drug well with very few side effects. Follow-up testing three months later shows the new drug is controlling his cancer, and he is feeling much better. The plan is to remain on this drug for as long as it is effective.
What is next for Carlos?
His oncologist explains that it is possible he could develop resistance to the second drug, but not to worry. New next-generation TRK inhibitors are being researched in clinical trials and he may qualify for one in the future. In addition, his blood and tissue will be retested at that time because there may be new molecular changes for which a different type of treatment may work.
*Carlos is not a real patient.