Colorectal Cancer
Staging
Doctors rely on many tests to diagnose colorectal cancer. Some tests, including laboratory studies and imaging studies such as computed tomography (CT), help doctors assign an initial stage to your cancer. This initial stage is known as the clinical stage because it is based on clinical findings. The final stage is assigned by the pathologist who examined the colon or rectal tumor and lymph nodes that were removed. This final stage is known as the pathologic stage. The stage provides important information for selecting treatment and for predicting the prognosis (outcome).
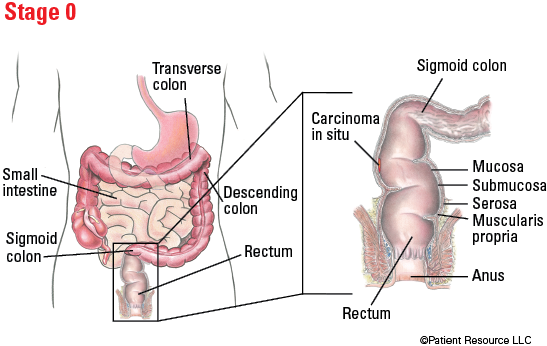
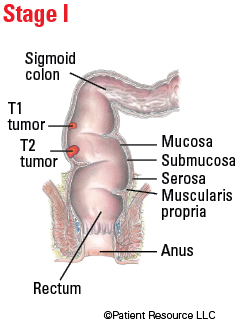
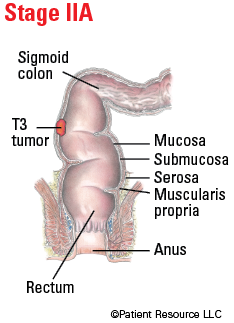
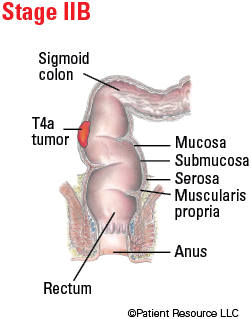
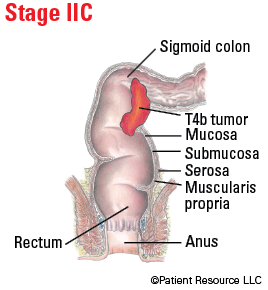
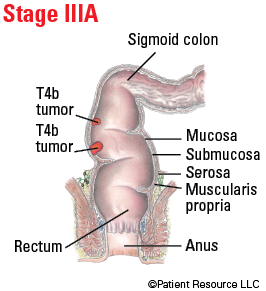
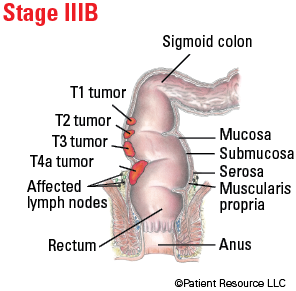
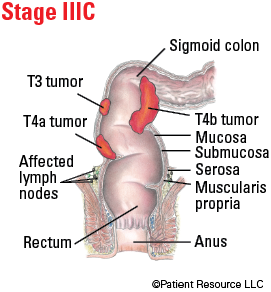
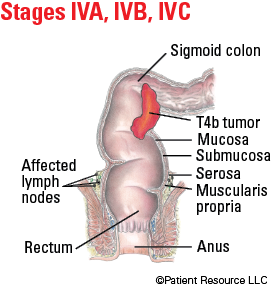
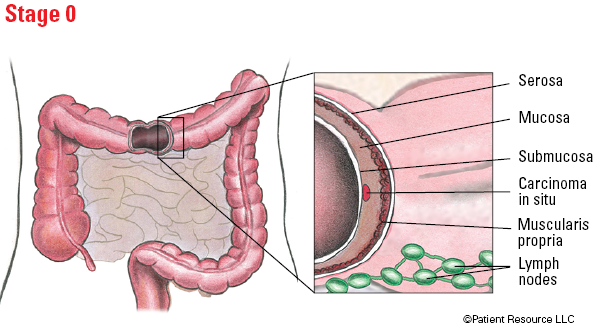
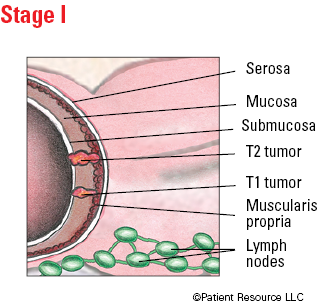
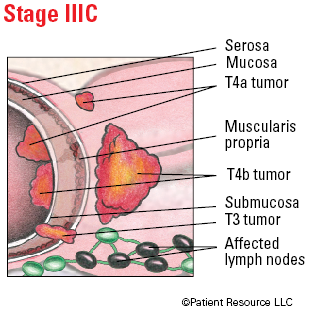
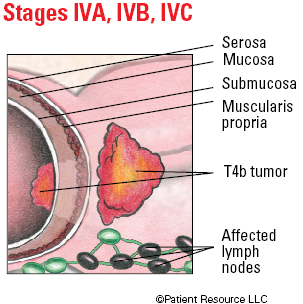
Colorectal cancer is classified according to the tumor, node, metastasis (TNM) system developed by the American Joint Committee on Cancer (AJCC). For many cancers, the size and location of the tumor is of critical importance, but for colorectal cancer, how deeply the tumor penetrates the intestinal or rectal layers is the most important feature of the tumor. The T category is used to describe this depth; the N category is used to describe how many nearby lymph nodes are involved (contain cancer cells); and the M category is used to note whether cancer has metastasized (spread to other parts of the body) (see Table 1).
Once a colorectal cancer has been classified with the AJCC TNM system, a prognostic stage group is assigned (see Table 2). Stages 0 to IV are further subdivided, grouping tumors that are associated with similar prognoses. This grouping enables doctors to more accurately predict the outcome according to the stage and to recommend the optimal treatment.
The stage of your colorectal cancer and other characteristics of the tumor are documented on a pathology report. A pathology report is prepared by a pathologist after he or she has examined the specimen with and without a microscope, documenting its size, describing its location and appearance, and performing special testing. Results from testing the tumor sample for mutations, also known as molecular testing, may be on the initial pathology report or reported later in a separate document. These results are important because they can help guide additional treatment decisions, such as which drug therapies to use, and identify people who need testing for Lynch syndrome, an inherited condition that results in a risk of developing colorectal and other cancers. Some commonly tested mutations in colorectal cancer are BRAF (pronounced BEE-raff) and RAS (pronounced Rass), which includes KRAS (pronounced KAY-rass) and NRAS (pronounced EN-rass), and EpCAM. Microsatellite instability (MSI) and deficient mismatch repair (dMMR) testing will likely be done, among others. Testing for HER2 overexpression is recommended for any patient with Stage IV colon cancer whose tumor does not have a RAS mutation.
Other important information about the tumor that is included on the pathology report includes its histologic grade and the status of the surgical margins. The histologic grade indicates how closely the tumor cells resemble healthy cells. Grade 1 cells look similar to healthy cells, and the tumor is likely to grow slowly; in contrast, Grade 4 cells look very different from healthy cells, and the tumor is likely to grow quickly. The surgical margin is the area of healthy tissue around the tumor. The pathologist will examine the margin to see if it contains cancer cells. If cancer cells are present in the margins, additional treatment may be needed.
An accurate diagnosis is crucial to receiving appropriate treatment. To gain more information, consider seeking a second opinion or advice from another doctor or group of doctors who specialize in treating colorectal cancer before or even after you begin treatment. Some doctors may favor one treatment approach, while others might suggest a different combination of treatments. You need to learn about all your treatment options. There is often collective wisdom gained from the experience and opinions of different oncology specialists who are experts in your type of cancer. A second opinion is also a way to make sure your pathology, diagnosis and staging are accurate and that you are aware of clinical trials that you might want to consider.
Table 1. AJCC TNM System for Classifying Colorectal Cancer
| Classification | Definition | |
| Tumor (T) | ||
| TX | Primary tumor cannot be assessed | |
| T0 | There is no evidence of primary tumor | |
| Tis | Carcinoma in situ, intramucosal carcinoma (involvement of lamina propria with no extension through muscularis mucosae). | |
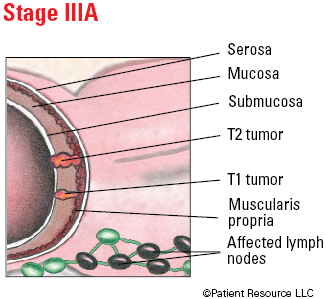
| T1 | Tumor invades submucosa (second layer of tissue in the colon or rectum)(through the muscularis mucosa [first layer of tissue in the colon or rectum] but not into the muscularis propria [third layer of tissue in the colon or rectum]). | |
| T2 | Tumor invades the muscularis propria (third layer of tissue in the colon or rectum). | |
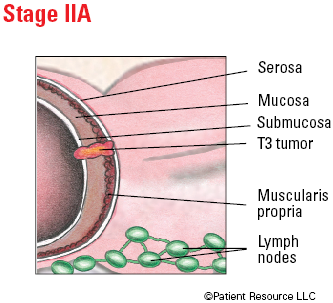
| T3 | Tumor invades through the muscularis propria (third layer of tissue in the colon or rectum) into pericolorectal tissues (tissues around the colon or rectum). | |
| T4 | Tumor invades the visceral peritoneum (outer lining of colon or rectum) or invades or adheres to adjacent organ or structure. | |
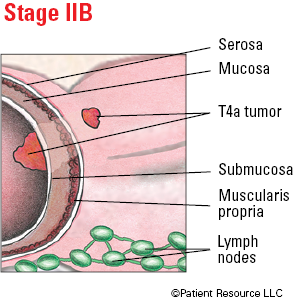
| T4a | Tumor invades through the visceral peritoneum (outer lining of colon or rectum) (including gross perforation of the bowel through tumor and continuous invasion of tumor through areas of inflammation to the surface of the visceral peritoneum). | |
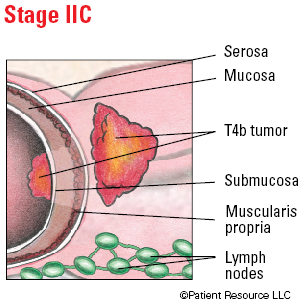
| T4b | Tumor directly invades or adheres to adjacent organs or structures. | |
| Node (N) | ||
| NX | Regional lymph nodes cannot be assessed. | |
| N0 | No regional lymph node metastases detected. | |
| N1 | One to three regional lymph nodes are positive (tumor in lymph nodes measuring greater than or equal to 0.2 mm), or any number of tumor deposits are present and all identifiable lymph nodes are negative. | |
| N1a | One regional lymph node is positive. | |
| N1b | Two or three regional lymph nodes are positive. | |
| N1c | No regional lymph nodes are positive, but there are tumor deposits in the subserosa, mesentery or nonperitonealized pericolic, or perirectal/mesorectal tissue (nearby tissues.) | |
| N2 | Four or more regional nodes are positive. | |
| N2a | >Four to six regional lymph nodes are positive. | |
| N2b | Seven or more regional lymph nodes are positive. | |
| Metastasis (M) | ||
| M0 | No distant metastasis by imaging, etc.: no evidence of tumor in distant sites or organs. | |
| M1 | Metastasis to one or more distant sites or organs or peritoneal (membrane that lines the abdominal cavity) metastasis is identified. | |
| M1a | Metastasis to one site or organ is identified without peritoneal (membrane that lines the abdominal cavity) metastasis. | |
| M1b | Metastasis to two or more sites or organs is identified without peritoneal (membrane that lines the abdominal cavity) metastasis. | |
| M1c | Metastasis to the peritoneal (membrane that lines the abdominal cavity) surface is identified alone or with other site or organ metastases. | |
Table 2. Stages of Colorectal Cancer
| Stage | T | N | M |
| 0 | Tis | N0 | M0 |
| I |
T1
T2 |
N0
N0 |
M0
M0 |
| IIA | T3 | N0 | M0 |
| IIB | T4a | N0 | M0 |
| IIC | T4b | N0 | M0 |
| IIIA |
T1-T2
T1 |
N1/N1c
N2a |
M0
M0 |
| IIIB |
T3-T4a
T2-T3 T1-T2 |
N1/N1c
N2a N2b |
M0
M0 M0 |
| IIIC |
T4a
T3-T4a T4b |
N2a
N2b N1-N2 |
M0
M0 M0 |
| IVA | Any T | Any N | M1a |
| IVB | Any T | Any N | M1b |
| IVC | Any T | Any N | M1c |
Illustrated Stages of Colon Cancer

Illustrated Stages of Rectal Cancer