HER2+ Breast Cancer
Reconstruction
When it is time to make decisions about reconstruction after a mastectomy, remember that it is an extremely personal decision that only you can make, and it is one that you should not rush. Before you make any decisions, learn about your options and think about what will make you most comfortable. Meet with a team experienced in breast reconstruction. Sometimes the initial stage of reconstruction can be done at the time of the mastectomy.
Many advocacy groups offer peer counseling so you can ask questions of women who have had reconstruction procedures. Ask your nurse/patient navigator for referrals. In addition, consider the following:
- Do your breasts play a crucial role in your personal sense of femininity and sexuality? If so, you may be eager to replace them to feel more like your pre-cancer self. That may involve reconstructive surgery, which includes flap reconstruction and implant-based reconstruction. If you are having a mastectomy or lumpectomy, your doctor will likely discuss breast reconstruction, which involves additional surgeries to restore or reshape one or both breasts. Reconstructive surgery is often performed, or at least started, during a mastectomy or can be delayed for a few months or even years. Mastectomy patients undergoing immediate reconstruction may be eligible for enhanced cosmetic approaches, such as skin-sparing or nipple-sparing mastectomy. Reconstruction may be done during or after a lumpectomy if the surgery will cause the affected breast to look significantly different from the other after the tumor is removed. Your plastic surgeon will work with you to set expectations for your new or reconstructed breast(s). It is important to realize that your breast(s) will not look or feel exactly as they did before or have the same sensation.
- Non-surgical options, such as breast prosthesis, are also available. Made from artificial materials, the prosthesis is designed to provide a natural, symmetrical appearance when you're dressed. You must wait until you're healed from surgery to be fitted for a prosthesis. One type is worn inside the hidden pocket of a mastectomy bra. Another type attaches to your body with a special adhesive, though this approach may not be recommended after chest wall radiation therapy. Mastectomy bras are available in many styles and colors. Many health insurance providers will cover the costs of a prosthesis and mastectomy bras if you provide a prescription from your oncologist or oncologic surgeon. Call your insurance provider to verify which mastectomy-related products are covered, the documentation required for reimbursement and how often you can purchase replacements.
- Not having reconstruction is an option you may not be aware of. This is often referred to as "going flat," which means not having a breast prosthesis, enhancement or additional surgery.
Questions to Ask Your Doctor
Deciding how to proceed before having any surgery allows your plastic surgeon to collaborate with your breast cancer surgeon during your mastectomy. To feel informed enough to make a decision, discuss your options with your doctors. These questions will get you started.
- Can I get this first stage of reconstruction done at the time of mastectomy?
- How soon will I be able to return to work or other important activities?
- If drains are necessary, how long will they stay in?
- Will the healing period required for breast reconstruction delay chemotherapy or interfere with post-mastectomy radiation?
- Am I a candidate for nipple- and areola-sparing mastectomy? Can you tell me more about nipple reconstruction and areola tattooing?
- Can you refer me to a peer-to-peer organization so I can learn about other women’s experiences?
Breast Reconstruction Options
Reconstructive Techniques
With an Implant A breast implant filled with silicone gel or saline (salt water) may sometimes be placed following the mastectomy in a single operation referred to as immediate reconstruction. In delayed reconstruction, a tissue expander is inserted under the skin following the mastectomy to gradually stretch the skin and underlying tissue; an implant is then placed in a second surgery, often when treatment is completed.
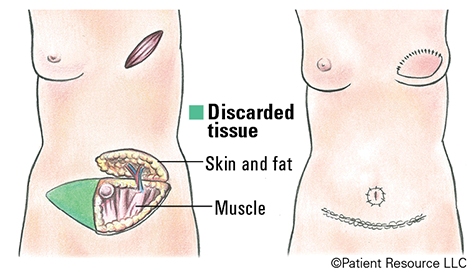
With a Tissue "FLAP" A tissue “flap” usually contains skin, fat, blood vessels and sometimes muscle. A pedicle flap remains attached to the body and is repositioned to the breast area with a muscle carrying the blood supply. A free flap is removed from the body along with blood vessels, which are then attached to the blood vessels in the breast area. Some types of flaps follow.
[DIEP] deep inferior epigastric perforator flap
[SIEA] superficial inferior epigastric artery flap
[TRAM] transverse rectus abdominis muscle flap
[LD] latissimus dorsi flap
[GAP] gluteal artery perforator flap (gluteal free flap)
[SGAP] superior gluteal artery perforator flap
[PAP] profunda artery perforator flap
[TUG] transverse upper gracilis flap
DIEP Flap Breast Reconstruction