HER2+ Breast Cancer
Treatment Planning
You are encouraged to take an active role in treatment planning. Share your goals and expectations with your doctor. For example, it may be essential that you have a treatment schedule that allows you to continue working, be actively involved in child care or family responsibilities, or participate in upcoming key life events. Breast cancer treatment will affect many aspects of your life, so now is the time to discuss the things that are most important to you.
About Breast Cancer Treatment
Local treatments, including surgery and radiation therapy, are focused on specific areas of the body. Systemic treatments – including drug therapies – travel throughout your body. Drug therapies can be given by injection, subcutaneously, orally or intravenously (IV) through a vein in your arm or through a port. You may choose to have a port surgically inserted under the skin in the upper chest area or arm to gain easy access to veins so you can receive the medicine without repeated needle sticks or risking damage to your veins.
Surgery is the most common option for many types of breast cancer. Drug therapy may be used when surgery is not an option.
Treatments are often referred to by when they are given. Treatment given before surgery is called neoadjuvant therapy. Treatment given after surgery is called adjuvant therapy. Whether delivered before or after surgery, an important goal of systemic therapy is to destroy breast cancer cells that may be hiding in other organs of the body, such as the liver, lungs, bones or brain. These hidden cancer cells, called micrometastatic disease, are usually too small to detect with laboratory testing or imaging studies. Delivering carefully selected systemic therapy to appropriate patients can often completely eliminate micrometastatic disease and is, therefore, extremely important as a partner with surgery for breast cancer to help a person become cancer-free.
Most people have more than one type of therapy, and treatment plans often change. The cancer may demonstrate resistance to the initial therapy by showing progression of disease, or it may appear to be under control and then grow back (recur) because of resistance. Either of these scenarios might prompt a change in your treatment plan. Sometimes a therapy will be modified to make side effects more tolerable. The good news is that when a change is necessary, there is almost always something else to try.
Types of treatment
Surgery is often the first treatment used for early-stage HER2+ breast cancers. Your doctor may choose to use chemotherapy and targeted therapy before an operation (neo-adjuvantly) if it is appropriate. At times, this is needed to evaluate the efficacy of the systemic therapy, make the tumor smaller, eliminate lymph node metastases, and/or determine the need for additional adjuvant therapy postoperatively. For metastatic cancer that has spread beyond axillary lymph nodes, surgery typically is used only to prevent or treat symptoms or complications.
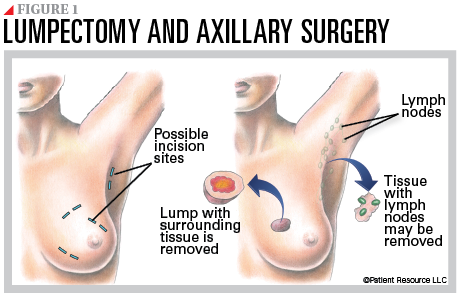
Lymph node surgery is usually necessary to either stage the cancer or to control cancer that is known to have spread to the nodes. The underarm (axilla) is the most important location for management of lymph nodes in breast cancer patients as it is the most common site for breast cancer to spread.
Most people undergo an initial staging procedure of their lymph nodes at the same time as their breast surgery. This staging procedure is called a sentinel lymph node biopsy. The sentinel node is the first node to which a cancer spreads. If the sentinel nodes contain a tumor, sometimes a more extensive operation to remove additional lymph node-bearing tissue from the underarm may be necessary, and this is called an axillary lymph node dissection (see Figure 1). As you discuss this part of your treatment plan, ask your doctor about strategies for this surgery that may reduce the risk of lymphedema, a common side effect of axillary dissection (see Supportive Care).
A lumpectomy removes the tumor along with a small margin of normal-appearing tissue around it (see Figure 1). It is used for early-stage breast cancers detected as small tumors, including Stages 0, I and II, and it is considered to be breast conserving or breast sparing (also referred to as a partial or segmental mastectomy).
A lumpectomy is usually followed by adjuvant breast radiation treatments designed to kill microscopic cancer cells hiding in other parts of the breast. If your tumor is relatively small and you wish to spare as much of your breast as possible, this surgical plan may be an option. Some patients are considered to be poor candidates for a breast-conserving lumpectomy because of abnormalities seen on their breast imaging (mammogram or ultrasound) or because of the inability to receive radiation treatment. It is also important that you discuss the likely cosmetic outcome of breast-conserving surgery with your doctor because surgery and radiation can cause some alteration to the shape of the breast.
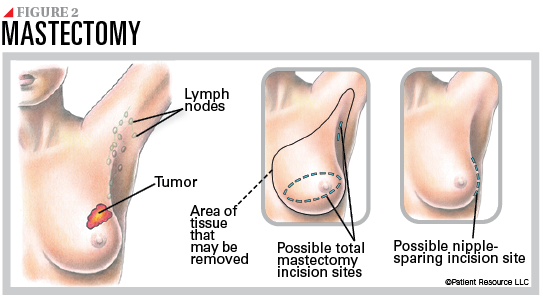
A mastectomy is the removal of the entire breast. It may be the preferred operation for patients with larger tumors, especially when they occur in a smaller breast (see Figure 2). Total mastectomy is the surgical removal of the entire breast without removing muscle. A modified radical mastectomy means that total mastectomy is being performed along with removal of a block of underarm/axillary lymph node tissue (axillary dissection). Skin-sparing and nipple-sparing mastectomies are alternative surgical approaches that may improve the cosmetic outcome of reconstruction.
At the end of the mastectomy procedure, drains are commonly placed into the area to collect fluid from the breast region. The incision is closed, and the area is covered by a bandage. You will be given information for incision and drain care, if applicable.
In certain instances, after the incisions have healed, outpatient radiation treatment to the breast is usually necessary after lumpectomy or even after mastectomy.
Drug therapy may include the following.
Targeted therapy is systemic therapy that uses drugs or other substances to identify and attack cancer cells by targeting sites on the cancer cells. Drugs that specifically treat HER2+ breast cancer are called anti-HER2 drugs. Designed to only attack the cancer cells, they include HER2 antibodies, HER2 antibody drug conjugates and HER2 inhibitors. Your doctor may prescribe more than one type of anti-HER2 drug at a time. Some may be given alone or in combination with other drug therapies. They may be used when surgery is not an option and as neoadjuvant, adjuvant or extended adjuvant therapy, which is designed to further reduce the risk of the cancer returning.
Chemotherapy drugs stop the growth of cancer cells by killing them or preventing them from dividing and growing. For early-stage HER2+ breast cancer, chemotherapy and HER2-targeted therapy may be given as a combination of two or three drugs or one after the other. For metastatic HER2+ breast cancer, chemotherapy is often combined with other anti-HER2 drugs.
Chemotherapy or targeted therapy or a combination may be used to shrink a tumor preoperatively so it can be surgically removed or to allow for a lumpectomy rather than a mastectomy. It may also permit you to avoid having an axillary dissection if nodal disease is eradicated. This approach has an advantage of helping your doctor determine how well the chemotherapy drugs work against the tumor. Chemotherapy is also given to destroy cancer cells that may remain after surgery, some of which may be too small to be detected with laboratory testing or imaging studies. This adjuvant systemic therapy is recommended for nearly all women with HER2+ breast cancer.
Hormone (endocrine) therapy may be prescribed if your disease is estrogen receptor positive (ER+) or progesterone receptor positive (PR+). Hormone therapy is designed to lower the amount of estrogen in your body or block the hormone receptors on the cancer cells.
Radiation therapy uses high-energy radiation to destroy cancer cells and shrink tumors. It may be necessary along with surgery. Sometimes it is given to control symptoms caused by breast cancer that has spread to specific organs, such as the bones or the brain.
Radiation therapy is usually recommended after a lumpectomy to destroy cancer cells that may remain hidden in normal-appearing breast tissue. Research shows that people with a small tumor who have radiation therapy after a lumpectomy live as long as those who have a mastectomy. Radiation therapy is sometimes necessary after a mastectomy and is typically recommended for individuals at high risk for cancer recurrence on the chest wall, such as those who have cancer in multiple axillary lymph nodes or a large cancer.
Clinical trials are research studies that may offer access to treatments, which are not yet widely available.
Maintenance
Even after successful treatment, breast cancer can recur (see Survivorship). To help prevent recurrence, maintenance medication or extended adjuvant therapy may be used. These drugs are typically taken for many months or years without stopping. Taking your medication as prescribed is critical. Talk with your health care team if you are unable to stay on schedule for any reason.
You will be monitored for signs of cancer with regular exams and blood tests. You will likely have mammograms of both breasts after a lumpectomy.
Exploring Reconstruction
If surgery is part of your treatment plan, you may want to pursue breast reconstruction. Learn more at PatientResource.com/HER2_Breast_Cancer_Reconstruction.
|
Commonly Drug Therapies for HER2 Breast Cancer
These therapies may be used alone or in combination. |
| Targeted Therapy |
| ado-trastuzumab emtansine (Kadcyla) |
| fam-trastuzumab deruxtecan-nxki (Enhertu) |
| lapatinib (Tykerb) |
| margetuximab-cmkb (Margenza) |
| neratinib (Nerlynx) |
| pertuzumab (Perjeta) |
| pertuzumab, trastuzumab and hyaluronidase-zzxf (Phesgo) |
| trastuzumab (Herceptin) |
| trastuzumab and hyaluronidase-oysk (Herceptin Hylecta) |
| tucatinib (Tukysa) |
| Hormone Therapy |
| anastrozole (Arimidex) |
| ethinyl estradiol |
| exemestane (Aromasin) |
| fluoxymesterone |
| fulvestrant (Faslodex) |
| goserelin acetate (Zoladex) |
| letrozole (Femara) |
| leuprolide acetate (Eligard, Lupron, Lupron Depot) |
| megestrol acetate (Megace) |
| tamoxifen |
| toremifene (Fareston) |
| Chemotherapy |
| capecitabine (Xeloda) |
| carboplatin (Paraplatin) |
| cisplatin |
| cyclophosphamide |
| docetaxel (Taxotere) |
| doxorubicin (Adriamycin) |
| epirubicin (Ellence) |
| eribulin (Halaven) |
| fluorouracil (5-FU) |
| gemcitabine (Gemzar) |
| ixabepilone (Ixempra) |
| liposomal doxorubicin (Doxil) |
| paclitaxel (Taxol) |
| protein-bound paclitaxel (Abraxane) |
| vinorelbine (Navelbine) |