Cancer Immunotherapy
Leukemia
Leukemia is a cancer that begins in abnormal blood cells within the bone marrow of both children and adults. Normal white blood cells help fight infection as part of the body’s immune system. When these cells become old or damaged, they die and are replaced with healthy new cells. But in leukemia, some of the white blood cells behave abnormally. They cannot fight infection properly, they grow uncontrollably and they don’t die when they should.
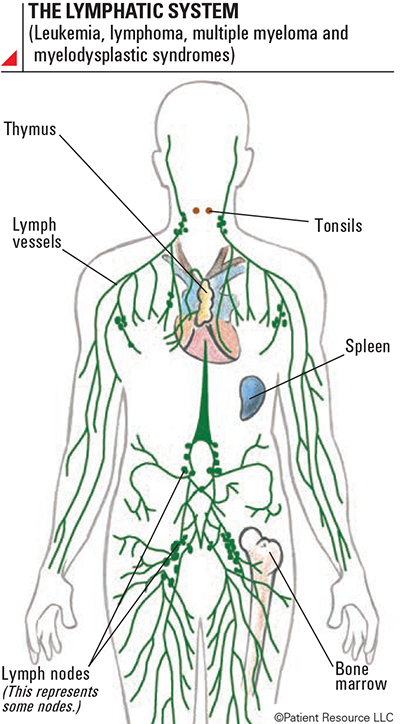
As a result, large numbers of the abnormal cells accumulate in the bone marrow, crowding out healthy blood cells and slowing or preventing new healthy cells from being produced. Unlike many other types of cancer, leukemia does not form solid tumors. Instead, when these abnormal cells continue to grow unchecked, the number of healthy white blood cells, red blood cells and platelets is reduced, putting the individual at increased risk of infection. As leukemia cells spill into the bloodstream, they travel to the lymph nodes, spleen, liver and elsewhere in the body, affecting normal body functions.
Leukemia is most often diagnosed in people older than 55, but it’s also the most common cancer diagnosed in children younger than 15.
Bone Marrow and Types of Blood Cells
Leukemia begins in the bone marrow, where blood is created, so knowing more about these important structures may help you better understand the disease (see Figure 1, below).
Bone marrow is the soft, spongy center of some bones. It contains immature blood stem cells, more developed blood-forming cells, fat cells and tissues that support cell growth.
Platelets are blood cells that gather around wounds, forming clots to stop the bleeding. They also help repair wounds and create blood vessels.
Red blood cells (erythrocytes) carry oxygen from the lungs to other parts of the body.
White blood cells (leukocytes) are essential to the immune system as the infection fighters of the body. There are several types of white blood cells. These two types are involved in leukemia:
- Lymphocytic cells (lymphocytes) make up lymphoid tissue found in the lymph nodes, thymus, spleen, tonsils and elsewhere in the body. Lymphocytes can be B-lymphocytes (B-cells), T-lymphocytes (T-cells) or natural killer (NK) cells.
- Myeloid (myelogenous) cells begin as immature blood stem cells that develop into red blood cells, white blood cells (excluding lymphocytes) and platelets.
Leukemia Blood Cells
More About Leukemia
Leukemia is classified by how rapidly the abnormal cells grow, the kind of blood cell in which the disease starts and its response to treatment.
Acute leukemia cells grow rapidly. They look similar to immature white blood cells, and as their numbers increase, the bone marrow is prevented from making normal, healthy blood cells.
Chronic leukemia cells look similar to healthy, mature white blood cells, but the cells are unable to mature fully. These leukemia cells grow slowly, and the progression of chronic leukemia varies from person to person.
Lymphocytic leukemia begins in bone marrow in cells that develop into white blood cells called lymphocytes. Lymphocytic leukemia is also sometimes called lymphoid or lymphoblastic leukemia.
Myeloid leukemia begins in early myeloid blood cells in the bone marrow. Myeloid leukemia is sometimes called myelogenous, myelocytic or myeloblastic leukemia.
Refractory leukemia is when leukemia cells are still present after some other treatment has been tried. Immunotherapy is available to treat some types of refractory leukemia. Your doctor will take into account the therapies you have already tried and your overall health before recommending another treatment plan.
Relapsed leukemia is the name given to leukemia that initially responds to treatment but stops responding after six months or more. Some types of leukemia have multiple relapses, which are also referred to as recurrences. If your cancer relapses, your doctor will begin a new cycle of diagnostic tests. These tests may include another tissue biopsy and laboratory tests. The doctor will confirm if the cancer is recurrent and determine if it has transformed into a more aggressive subtype, which will affect your new treatment plan.
Immunotherapy for Leukemia
Each type of leukemia responds differently to various therapies, so your medical team will recommend treatment options based on your type of leukemia and other factors, including your age, overall health and prognosis (predicted outcome from treatment) (see the Lymphatic System). It is important to learn as much as possible about your diagnosis and the available options so you can confidently partner with your medical team to make treatment decisions and manage your disease.
Following are the types of immunotherapy that are approved to treat various forms of leukemia. One or a combination of treatments may be used with immunotherapy, including chemotherapy, targeted therapy and stem cell transplantation. A variety of options continue to be researched for leukemia and other cancers in clinical trials.
A form of adoptive cellular therapy (T-cell therapy) called chimeric antigen receptor (CAR T-cell) therapy is approved to treat children and young adults who have B-cell precursor acute lymphocytic leukemia (ALL). Research in clinical trials continues to explore CAR T-cell therapies alone and in combination with other drugs for certain types of leukemia and other cancers.
A cytokine in the form of interferon is approved to treat chronic myeloid leukemia (CML) although it is not typically used as a first-line treatment.
Monoclonal antibodies are approved to treat certain types of leukemia, used alone or in combination with other therapies.
An immunomodulator may be used alone or in combination with other therapies to treat certain leukemia diagnoses.