Multiple Myeloma
Treatment Planning
Breakthroughs in understanding multiple myeloma are revolutionizing treatment strategies, with new treatment options that may enable physicians to manage it as a chronic disease. To develop the most effective plan, you and your doctor will determine your specific goals.
Reaching remission is the primary goal of treating multiple myeloma. Remission means no longer having any signs or symptoms of the disease.
Your treatment plan may include therapies designed to eliminate myeloma cells, control tumor growth, minimize and manage pain, and focus on enabling you to enjoy your desired quality of life. Your doctor will consider the following:
- The stage of the disease
- Whether it is a new diagnosis or a recurrence
- The presence of symptoms
- The aggressiveness of the disease
- Previous treatments
- Previous treatments
- Your age and overall health
Treatment Options
Several treatment strategies may be recommended, sometimes with more than one being used at the same time. Using several drugs together, called doublet, triplet or quadruplet therapy depending on the number of drugs being used, helps prevent resistance, a condition in which the disease stops responding to therapy.
It is a good idea to be familiar with the different available options because regardless of the plan you begin with, your strategy may change. Your doctor may continually monitor your condition and make adjustments for a number of reasons, such as resistance. The overall goal is to give you the best level of care possible.
Watchful waiting may be recommended for people with monoclonal gammopathy of undetermined significance (MGUS) or smoldering myeloma (early-stage disease), and when symptoms are not present. It offers the possibility of delaying active treatment and avoiding the side effects of treatment as long as possible. It is very important to make and keep regular checkups because treatment should begin as soon as the disease progresses or symptoms appear.
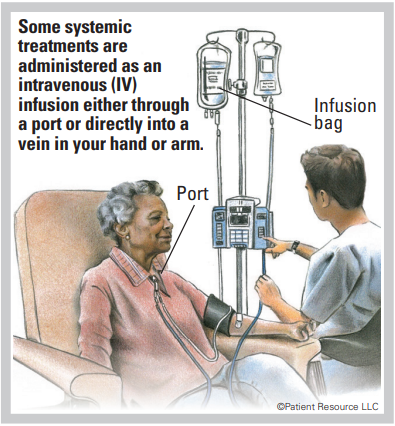
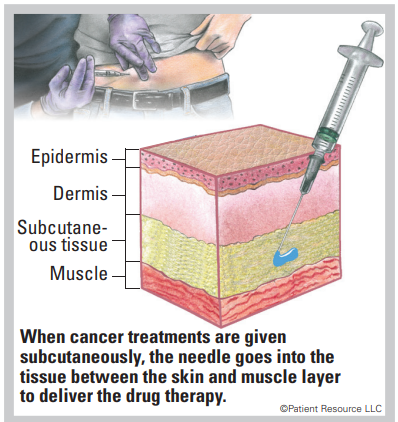
Drug therapies are frequently used to treat multiple myeloma. They are systemic therapies, which means they travel throughout the body. They may be delivered orally, intravenously or subcutaneously by injection under the skin.
Chemotherapy is commonly given to people with multiple myeloma. It is designed to destroy cancer cells. It may consist of a single drug or multiple drugs given in combination, and it may be combined with other types of treatment. Chemotherapy is sometimes given in high doses to destroy myeloma cells before a stem cell transplant. Some oral chemotherapy drugs may be taken at home. Intravenous (IV) drugs are given in a doctor’s office, clinic or hospital.
Corticosteroids are myeloma cell-fighting drugs that may also ease chemotherapy side effects, particularly nausea and vomiting. They can be used alone or in combination with chemotherapy. Corticosteroids also help reduce inflammation and may offer other benefits.
Immunotherapy works with your immune system to help identify and then destroy multiple myeloma cells. It may be given in a doctor’s office, clinic or hospital by IV or subcutaneously by injection.
Immunotherapy comes in different forms:
- Monoclonal antibodies (mAbs) are made to target specific antigens — in this case, ones found on myeloma cells. The mAbs can be made to recognize and attach to proteins and other substances on multiple myeloma and other cells or deliver other therapeutic agents to slow their growth and/or kill them. They might also enable your immune system to learn to identify and destroy multiple myeloma cells.
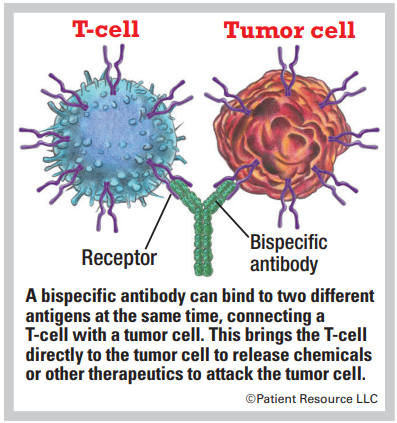
- Bispecific mAbs are made up of two different mAbs that can attach to two different antigens at the same time and can be delivered without removing a patient’s immune cells. They can be used for engaging and activating immune cells, such as T-cells, to attack a tumor. Many of these are known as bispecific T-cell engagers (BiTEs).
- Chimeric antigen receptor (CAR) T-cell therapy involves taking a patient’s T-cells and modifying them to recognize and kill multiple myeloma cells (see CAR T-cell Therapy).
Targeted therapy attacks certain cancer cells and avoids healthy cells, resulting in fewer side effects than traditional chemotherapy. These drugs may be given orally (at home), subcutaneously or by IV (in a doctor’s office, clinic or hospital). They travel throughout the body via the bloodstream looking for specific proteins and tissue environments of myeloma cells.
The following types of targeted therapy drugs may be used alone or in combination:
- Angiogenesis inhibitors block new blood vessel growth that feeds myeloma cells.
- BCL-2 inhibitors block the BCL-2 protein, which is found in myeloma cells.
- Histone deacetylase (HDAC) inhibitors affect gene expression inside myeloma cells.
- Immunomodulators may stimulate or slow down the immune system in indirect ways. They may boost the immune system and the effects of other therapies on the myeloma cells. They may be effective in treating newly diagnosed multiple myeloma and relapsed or refractory disease.
- Monoclonal antibodies (mAbs) are commonly used. Laboratory-made mAbs attach to specific proteins and attack myeloma cells. These are also often discussed as a type of immunotherapy.
- Bispecific mAbs, which are also categorized as a type of immunotherapy, are made up of two different mAbs that can attach to two different antigens at the same time and can be delivered without removing a patient’s immune cells.
- Proteasome inhibitors target enzymes to slow or stop myeloma cell growth and development.
- Selective inhibitors of nuclear export (SINE) enhance the anti-cancer activity of certain proteins in a cell.
Bone-modifying (strengthening) drugs are used to treat bone problems caused by multiple myeloma as well as prevent further bone damage from occurring. Contact your doctor as soon as you begin to feel any pain.
Systemic Therapy
Subcutaneous Injection
Bispecific Antibody
Stem cell transplantation may be part of your treatment plan (see Stem Cell Transplantation). This therapy infuses healthy blood stem cells into the patient to restore the body’s ability to produce enough healthy new blood cells. An autologous (auto) transplant using the patient’s own stem cells may be done when treating multiple myeloma. An allogeneic (allo) transplant may be an option for patients with a high risk of relapse, those who are not responding fully to other treatments or those who have relapsed disease. This type of transplant uses donor cells, which are collected from a family member or an unrelated donor.
Radiation therapy may be used for localized myeloma or bone pain that does not lessen with chemotherapy.
Surgery may be used to treat a plasmacytoma (malignant plasma cell tumor), but it is rarely a treatment option. In cases of weakened bone, metal plates or rods may be placed surgically to provide support or to prevent fractures.
Plasmapheresis, though not a treatment specifically for multiple myeloma, may be needed if large amounts of M-protein make the blood too thick. It involves using a machine to filter M-proteins out of the plasma.
Clinical trials offer the opportunity to try an innovative treatment being tested for multiple myeloma patients before being widely available (see Clinical Trials).
Ongoing Monitoring
To evaluate the effectiveness of your treatment and determine that the disease has not developed resistance to the medications, your doctor will monitor your treatment and health status on a regular basis using different methods.
CRAB – Your doctor will run blood and imaging tests that are helpful in detecting CRAB, the common signs of multiple myeloma (see Introduction, page 5).
MRD – Your doctor may use measurable/minimum residual disease (MRD) testing. MRD is used to describe a very small number of cancer cells that remain in the body during or after treatment. It can be found only by highly sensitive laboratory methods that are able to find one cancer cell among one million normal cells. Checking for MRD may identify appropriate treatment, determine how well treatment is working, detect whether cancer has come back or make a prognosis.
When residual cancer cells are still detectable in the blood, this is known as being “MRD positive.” When no cancer cells can be found, it is known as being “MRD negative.” Research studies have shown that MRD negativity is associated with longer remissions.
Because of the progress surrounding multiple myeloma treatments, a patient may have a very long remission that might be referred to as a “durable response.” A durable response is typically seen with immunotherapy drugs.
COMMON DRUG THERAPIES FOR MULTIPLE MYELOMA
These therapies may be used alone or in combination.
| Drug Therapies For Multiple Myeloma |
| bortezomib (Velcade) |
| carfilzomib (Kyprolis) |
| ciltacabtagene autoleucel (Carvykti) |
| carmustine (BiCNU) |
| cyclophosphamide |
| daratumumab (Darzalex) |
| daratumumab and hyaluronidase-fihj (Darzalex Faspro) |
| dexamethasone |
| doxorubicin hydrochloride (Adriamycin) |
| doxorubicin liposomal (Doxil) |
| elotuzumab (Empliciti) |
| elranatamab-bcmm (Elrexfio) |
| idecabtagene vicleucel (Abecma) |
| isatuximab-irfc (Sarclisa) |
| ixazomib (Ninlaro) |
| lenalidomide (Revlimid) |
| melphalan (Alkeran) |
| panobinostat (Farydak) |
| pomalidomide (Pomalyst) |
| prednisone |
| selinexor (Xpovio) |
| talquetamab-tgvs (Talvey) |
| teclistamab-cqyv (Tecvayli) |
| thalidomide (Thalomid) |
| Some Possible Combinations |
| carfilzomib (Kyprolis) with dexamethasone or lenalidomide (Revlimid) plus dexamethasone |
| carmustine (BiCNU) with prednisone |
| daratumumab and hyaluronidase-fihj (Darzalex Faspro) with bortezomib (Velcade) and dexamethasone |
| daratumumab and hyaluronidase-fihj (Darzalex Faspro) with bortezomib (Velcade), melphalan and prednisone |
| daratumumab and hyaluronidase-fihj (Darzalex Faspro) with bortezomib (Velcade), thalidomide (Thalomid) and dexamethasone |
| daratumumab and hyaluronidase-fihj (Darzalex Faspro) with lenalidomide (Revlimid) and dexamethasone |
| daratumumab and hyaluronidase-fihj (Darzalex Faspro) with pomalidomide and dexamethasone |
| daratumumab (Darzalex) with lenalidomide (Revlimid) and dexamethasone |
| daratumumab (Darzalex) with bortezomib (Velcade), melphalan (Alkeran) and prednisone |
| daratumumab (Darzalex) with bortezomib (Velcade), thalidomide (Thalomid) and dexamethasone |
| daratumumab (Darzalex) with bortezomib (Velcade) and dexamethasone |
| daratumumab (Darzalex) with pomalidomide (Pomalyst) and dexamethasone |
| elotuzumab (Empliciti) with lenalidomide (Revlimid) and dexamethasone |
| elotuzumab (Empliciti) with pomalidomide (Pomalyst) and dexamethasone |
| isatuximab-irf (Sarclisa) with pomalidomide (Pomalyst) and dexamethasone |
| isatuximab-irfc (Sarclisa) with carfilzomib and dexamethasone |
| ixazomib (Ninlaro) with lenalidomide (Revlimid) and dexamethasone |
| lenalidomide (Revlimid) with dexamethasone |
| liposomal doxorubicin (Doxil) with bortezomib (Velcade) |
| panobinostat (Farydak) with bortezomib (Velcade) and dexamethasone |
| pomalidomide (Pomalyst) with dexamethasone |
| selinexor (Xpovio) with dexamethasone |
| thalidomide (Thalomid) with dexamethasone |
Relapsed and refractory multiple myeloma
Multiple myeloma is frequently treated like a chronic condition that can return. Regardless of how many times it returns, the primary goal of treating it is to reach remission.
Complete remission is reached when cancer can no longer be found after multiple tests. However, even with complete remission, small numbers of cancer cells may still be in the body. That is called a partial remission, and it occurs when some but not all signs and symptoms have decreased or disappeared.
Disease that comes back after treatment is called relapsed myeloma. A relapse can happen weeks, months or even years after initial treatment has ended. Staying on schedule with follow-up appointments is important because noticing a recurrence early is key to more successful treatment.
Refractory myeloma occurs when the cancer no longer responds to treatment. The disease may not respond to initial therapy or may stop responding after treatment has been underway for a length of time. If this happens, your doctor may request additional tests and re-staging may occur. If a new stage is assigned, your treatment options will likely change.
The importance of medication adherence
Most cancer therapies are designed to maintain a specific level of drugs in your system for a certain time based on your cancer type and stage, your overall health, previous therapies and other factors. If your medications are not taken exactly as prescribed, or if you miss appointments for your infusions, injections or radiation therapy, the consequences can be serious, even life-threatening. To be fully effective, every treatment dose must be taken with the same kind of accuracy, precise timing and safety precautions, for as long as prescribed. This is known as medication adherence.