Radiation Therapy
Radiation Therapy Options
When developing your treatment plan, your radiation oncologist considers many factors to select the best radiation therapy for you. Important factors include the type of cancer, the size of the tumor, the location of the tumor, how close the treatment area is to normal tissues, how far the radiation has to travel, your general health and medical history and any other cancer treatments you may receive. You may have radiation therapy that is intended to help cure your cancer or to help manage the pain caused by your cancer.
High-energy X-rays and charged particles are types of radiation often used for cancer treatment. X-rays for radiation therapy are many times more powerful than X-rays used for diagnostic imaging (such as a chest X-ray).
There are three categories of radiation: external, internal and systemic.
External-beam radiation therapy
External-beam radiation therapy (EBRT) is the most frequently used type of radiation therapy. In EBRT, the radiation comes from a machine outside the body. These machines are called linear accelerators and they direct the radiation, most often photon beams (high-energy X-rays), to the tumor. EBRT can also be delivered with electron beam radiation, which has similar effects as photons but with different dose shaping capabilities. EBRT does not make a patient radioactive.
EBRT can be used to treat large areas of the body and more than one area (for example, the main tumor and lymph nodes near it). Even though the radiation is aimed at the cancer, it can affect the normal tissue it travels through on its way into and out of the body. External-beam radiation therapy can be administered in many ways.
Three-dimensional conformal radiation therapy
Three-dimensional conformal radiation therapy (3D-CRT) is a common form of EBRT. It involves the use of special computer software and treatment machines to create a three-dimensional image of the tumor. The image lets the doctors direct the highest possible dose of radiation to the tumor while affecting the healthy tissue as little as possible.
Intensity-modulated radiation therapy
Intensity-modulated radiation therapy (IMRT) is a sophisticated type of EBRT. Like 3D-CRT, it also involves the use of software to create a precise, three-dimensional image of the tumor. These images are then used to shape the radiation beams to target the tumor more precisely. It is also possible to adjust the strength, or intensity, of the beams. Changing the intensity gives more control of the dose and lets the doctor deliver high amounts of radiation to the tumor while giving less radiation to normal tissue.
Volumetric modulated arc therapy (VMAT) is a kind of IMRT. For VMAT, the treatment machine rotates quickly around the patient at least once, shaping and reshaping the radiation beam continually to match the shape, size, and position of the tumor. This rapid rotation means that each treatment lasts just a few minutes. This type of radiation therapy can be more convenient for the patient because it delivers radiation faster than some other types.
Image-guided radiation therapy
Image-guided radiation therapy (IGRT) is an option on radiation machines with imaging capabilities built into them. The scanners may be used to obtain diagnostic X-rays or computed tomography (CT) images. These built-in scanners let the doctor take pictures of the tumor to track any changes in a tumor’s size or location. If necessary, the doctor can then make minor aiming adjustments, which may make radiation delivery even more precise.
Because machines with IGRT technology can create an image of the tumor right before treatment sessions, they can target the tumor precisely, while sparing healthy tissue.
Stereotactic radiosurgery
Stereotactic radiosurgery (SRS) uses thin beams of radiation given from many angles to provide a large dose of radiation to a small tumor area very quickly (often in a single session). Even though it is called surgery, it is a kind of radiation therapy and is non-invasive because no scalpel is used.
SRS uses the exact location of the tumor as shown on CT or MRI scans and requires that the patient is positioned precisely. Because of this, SRS can deliver radiation without excess damage to normal cells nearby. It is used to treat small tumors of the brain or spine, including brain metastases. A head frame or shell may be used to keep the patient’s head in place.
Stereotactic body radiation therapy
Stereotactic body radiation therapy (SBRT) is similar to SRS. It precisely delivers radiation to tumors in the body that are not in the brain or spinal cord. Because these tumors are more likely to move with the patient’s normal movements, these treatments require special technology for localizing the tumor through imaging and then compensating for any tumor or patient motion. SBRT is used to treat small, isolated tumors, such as those in the lung or liver. A body frame is often used to align the patient for treatment, and organ movement, due to functions such as breathing, may be monitored to ensure that the treatment remains accurate.
Proton therapy
The EBRT techniques already listed deliver radiation by photon beams. Protons are a type of charged particle that can also be used to deliver radiation. The main difference between protons and photon beams is how they deposit energy in living tissue. Photons deposit energy in small amounts along their entire path through the tissue. In contrast, protons deposit a lot of their energy at the end of their path, leaving less along their way through the tissue.
This difference means that protons may reduce the amount of radiation deposited in normal tissue. It also suggests that protons may be able to deliver high doses of radiation to a tumor. However, more studies are needed to confirm this.
The machine that delivers proton therapy is not yet widely available.
Other charged particle beams
Electron beams can be used to treat superficial tumors, such as skin cancer or tumors near the surface of the body. Electron beams cannot travel far through the tissue, so they cannot treat tumors deeper in the body.
Internal radiation therapy (Brachytherapy)
For internal radiation therapy, or brachytherapy, sources of radiation are placed in or near the area to be treated. Because the radiation travels just a short distance, the risk of damaging normal tissue is lower than with EBRT. Brachytherapy can be a good option for tumors that require a high dose of radiation or are near sensitive normal tissues that are easily damaged by radiation.
Depending on where it is placed, brachytherapy may be intracavitary or interstitial. In intracavitary radiation, the radioactive material is placed in a body cavity, such as the rectum, uterus or cervix. The cavity may also be one that results from surgery, such as the space left in the breast after a lumpectomy (see Figure 1). In interstitial radiation, the radioactive source is placed in or near the tumor using needles or catheters, but not in a body cavity.
Brachytherapy placement can be permanent or temporary.
In permanent brachytherapy, seeds or pellets of radioactive material are placed in the tumor with a needle (see Figure 2). The seeds are about the size of a grain of rice. Once in place, they give off radiation for a few weeks or months and are left in place after the radioactive material is used up. During permanent brachytherapy, the patient is temporarily radioactive, but the amount of radiation that reaches the surface of the skin is very low. Still, contact with pregnant women and young children may be restricted for a certain amount of time.
In temporary brachytherapy, cylinders, needles, catheters or balloons are placed in the treatment area. Radioactive materials are placed in these containers, left for a short time and then removed. Temporary brachytherapy can be administered at a high-dose rate (HDR) or a low-dose rate (LDR).
In HDR brachytherapy, the radiation source is placed for a few minutes at a time and then removed. Schedules will vary with treatment plans, but the process can be repeated twice a day for up to a week or once a week for a few weeks. In LDR brachytherapy, the radioactive material stays in place for up to seven days. To keep the radiation source from moving, patients must stay in bed. Because of this, patients receiving LDR therapy stay in the hospital.
During temporary brachytherapy, the patient is radioactive as long as the radioactive material is inside the patient’s body. As soon as it is removed, the patient is no longer radioactive. Because of this, patients receiving temporary brachytherapy usually stay in the hospital in a special room that protects other people from the radiation.
Figure 1: Temporary Brachytherapy
Breast Example
Temporary radioactive source (seeds) is placed in the breast through a catheter into a device.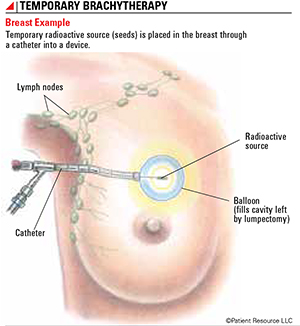
Figure 2: Permanent Brachytherapy
Prostate Example
Permanent radioactive seeds are placed in the prostate with a needle.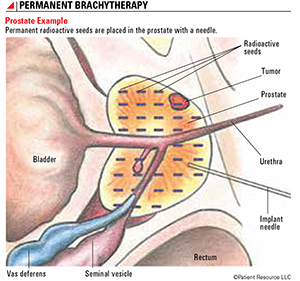
Systemic radiation therapy
EBRT and brachytherapy both target the specific location of the tumor. In contrast, systemic radiation treats the entire body. In systemic radiation therapy, a patient swallows a radioactive substance (a pill or a tasteless solution in water) or receives it as an injection.
Radioactive iodine is used to treat some kinds of thyroid cancer. For some other types of cancer, systemic radiation therapy may be administered as a drug with a monoclonal antibody that helps direct the radioactive material to the tumor. For example, ibritumomab tiuxetan (Zevalin) is used to treat certain types of B cell non-Hodgkin lymphoma. Other systemic radiation therapy drugs for other cancer types are being studied in clinical trials.
Some systemic radiation therapy drugs relieve pain caused by cancer that has spread to the bone (bone metastasis). These drugs are called radiopharmaceuticals. Samarium-153 lexidronam (Quadramet) and strontium-89 chloride (Metastron) are two radiopharmaceuticals that treat pain caused by bone metastasis.
Some types of systemic radiation therapy may make a patient’s body fluids temporarily give off a low level of radiation. Patients may need to limit contact with others, especially avoiding contact with children younger than 18 years and pregnant women.
Q & A With Your Treatment Team
When you consider radiation therapy as part of your treatment plan, it is important to learn as much as you can about all of your options before making a decision. Be honest with your treatment team about any concerns you may have and don’t be afraid to ask questions that will help you determine if radiation is right for you. To get you started, here are answers to some of the most commonly asked questions.
Question: If I’ve already had surgery to remove my cancer, why would radiation be necessary?
Answer: The goal of radiation therapy given after primary surgical treatment is typically to destroy any cancer cells that may remain. Even if a surgeon believes the entire tumor and any cancerous lymph nodes have been successfully removed, there is a chance that undetectable cancer cells may still exist and begin to grow again. Radiation to the surgical site can lower the risk of recurrence by destroying those cells that could potentially remain. The type of radiation used will depend on your diagnosis.
Question: Am I a candidate for different types of radiation? Am I being treated with the most advanced technology for my needs?
Answer: Several different types of radiation therapy are available. When you consider radiation as a treatment option, it is important to know which types of radiation are appropriate for you and whether your treatment center offers the latest technology. Talk to your doctor about all of your options and look for resources specific to a certain type of therapy. Getting a second opinion may be valuable to help you determine which radiation therapy option has the most potential benefit to you.
Question: When and how will I know if radiation was successful?
Answer: Radiation therapy does not kill cancer cells immediately. When a cell is unable to repair the DNA damage caused by the radiation, it dies. It could take days or weeks of treatment before this happens and the tumor begins to shrink. Then, the tumor may continue to shrink for weeks or months after radiation therapy ends. Your doctor may monitor progress with diagnostic testing.
If you are receiving radiation therapy after primary surgical treatment, the radiation is targeted at undetectable cells that may remain in the surgical site. Because you are unable to see or detect the cancer cells to begin with, you may not be able to determine the effectiveness of treatment right away. You will likely receive follow-up care after radiation ends to monitor for recurrence.
Question: Why do radiation oncologists and therapists take so many safety precautions for themselves while giving me my radiation treatments?
Answer: If you have chosen radiation as part of your treatment plan, the appropriate radiation dose will be calculated according to several factors and then divided among the appropriate number of treatments. As a patient, you are likely receiving only one series of treatments to a specific area. Radiation specialists, however, work with several patients every single day, often for years. Staff is required to follow specific protocol (such as leaving the room during external-beam radiation or wearing protective gear while providing internal or systemic radiation) when delivering radiation as a safety precaution. These precautions are set in place to protect professionals that work in the radiation clinic.
Question: If radiation is dangerous, why is it used to treat cancer?
Answer: As with any cancer treatment, it is important to consider the benefits versus the risks of that particular option. If your treatment team recommends radiation, it means they believe that the benefits are anticipated to outweigh the risks.
Radiation works by causing DNA damage within the cells. Healthy tissue has a greater ability to repair this damage compared to most tumor cells. The accumulation of damage within tumor cells eventually becomes lethal. Radiation can cause injury to some of the normal cells, but severe toxicity to normal organs resulting from this injury is unusual. However, some of this damage can be long-lasting so it is very infrequent to receive two courses of radiation to the same area of the body. Your radiation oncologist should help you understand the risks and benefits of radiation treatments so that you can contribute to decisions about your treatment.
Recent advancements in radiation techniques allow for better control of the radiation doses and more precise delivery to the treatment site, which minimizes radiation exposure to healthy tissue. This often means fewer side effects. If side effects are experienced, they are typically limited only to the area of the body being irradiated.