Ovarian Cancer
Overview and Staging
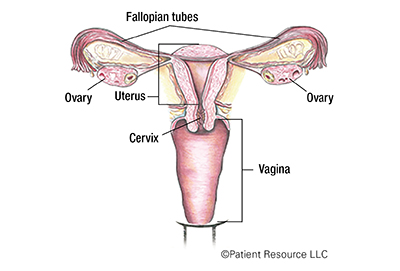
Ovarian cancer forms in the ovaries, which produce eggs and are the main source of the female hormones estrogen and progesterone. The eggs travel from the ovaries through the fallopian tubes into the uterus. Women have two ovaries, one on each side of the uterus.
There are three types of ovarian cancer. Each is named for the type of cell where it began:
- Epithelial carcinomas begin in the cells that line the outer surface of the ovaries. It is the most common type of ovarian cancer.
- Germ cell tumors originate in the egg-producing cells of the ovaries.
- Stromal cell tumors start in the connective tissue cells that hold the ovaries together and produce hormones.
Fallopian tube cancer, the rarest gynecologic cancer, is related to ovarian cancer. Some researchers think that ovarian cancer actually starts in the fallopian tubes. Treatment for fallopian tube cancer is often the same as that for ovarian cancer.
Diagnosing and staging
To diagnose ovarian cancer, your doctor will perform a physical exam and may order imaging tests. A biopsy is the only way to definitively diagnose ovarian cancer. Some of the tests done to diagnose your cancer will also help your doctor stage it. Staging cancer refers to determining the extent of cancer based on the size of the tumor and whether it has spread (and, if so, how far).
The staging process for ovarian cancer depends on several factors. It is based on results of physical examinations, imaging tests and the evaluation of surgically removed tissue samples. Knowing your stage helps you and your health care team choose the best treatment option for you.
To determine how far the cancer cells have spread, your surgeon might remove nearby lymph nodes, tissue and fluid within the pelvic and/or abdominal cavity for microscopic observation. The pathologist’s review of these samples will help determine an accurate stage, which is essential in establishing the most effective treatment plan for your specific type and stage of ovarian cancer.
Ovarian cancer is classified according to the tumor, node, metastasis (TNM) system developed by the American Joint Committee on Cancer. The tumor (T) is categorized according to its size and location, whether cancer cells are found in nearby lymph nodes (N), and whether cancer has metastasized (M) or spread to other parts of the body. Once an ovarian cancer has been classified with this system, an overall stage is assigned (see Staging Illustrations).
Table 1. TNM Ovarian Cancer Classifications
| Classification | Definition |
| Tumor (T) | |
| TX | Primary tumor cannot be assessed. |
| T0 | No evidence of primary tumor. |
|
T1
T1a
T1b T1c T1c1 T1c2
T1c3
|
Tumor limited to ovaries (one or both).
Tumor limited to one ovary (capsule intact), no tumor on ovarian surface; no malignant cells in ascites (abdominal fluid) or peritoneal washings (procedure to wash peritoneal cavity, remove the fluid and check for cancer cells).
Tumor limited to both ovaries (capsules intact); no tumor on ovarian surface; no malignant cells in ascites (abdominal fluid) or peritoneal washings (procedure to wash peritoneal cavity, remove the fluid and check for cancer cells).
Tumor limited to one or both ovaries, with any of the following:
Surgical spill (tissue surrounding tumor broke during surgery, which could allow cancer cells to leak into the abdomen or pelvis).
Capsule ruptured (tissue around tumor burst) before surgery or tumor on ovarian surface.
Malignant cells in ascites (abdominal fluid) or peritoneal washings (procedure to wash peritoneal cavity, remove the fluid and check for cancer cells).
|
|
T2
T2a
T2b
|
Tumor involves one or both ovaries with pelvic extension below pelvic brim.
Extension and/or implants on the uterus and/or fallopian tube(s).
Extension to and/or implants on other pelvic tissues.
|
|
T3
T3a T3b T3c |
Tumor involves one or both ovaries, with microscopically confirmed peritoneal metastasis outside the pelvis and/or metastasis to the retroperitoneal (pelvic and/or para-aortic (lymph nodes along the aorta)) lymph nodes.
Microscopic extrapelvic (above the pelvic brim) peritoneal involvement with or without positive retroperitoneal lymph nodes.
Macroscopic peritoneal metastasis beyond pelvis 2 cm or less in greatest dimension with or without metastasis to the retroperitoneal lymph nodes.
Macroscopic peritoneal metastasis beyond the pelvis more than 2 cm in greatest dimension with or without metastasis to the retroperitoneal lymph nodes (includes extension of tumor to capsule of liver and spleen without parenchymal involvement of either organ).
|
| Node (N) | |
| NX | Regional lymph nodes cannot be assessed. |
| N0 | No regional lymph node metastasis. |
| N0(i+) | Isolated tumor cells in regional lymph node(s) no greater than 0.2 mm. |
|
N1 N1a N1b |
Positive retroperitoneal lymph nodes only (histologically confirmed). Metastasis up to and including 10 mm in greatest dimension. Metastasis more than 10 mm in greatest dimension. |
| Metastasis (M) | |
| M0 | No distant metastasis. |
|
M1 M1a M1b |
Distant metastasis, including pleural effusion (metastasis to fluid in the lungs) with positive cytology; liver or splenic parenchymal metastasis; metastasis to extra-abdominal organs (including inguinal lymph nodes and lymph nodes outside the abdominal cavity); and transmural involvement of intestine. Pleural effusion (metastasis to fluid in the lungs) with positive cytology. Liver or splenic parenchymal metastases; metastases to extra-abdominal organs (including inguinal lymph nodes and lymph nodes outside the abdominal cavity); transmural involvement of intestine. |
Table 2. Stages of Ovarian Cancer
| Stage | TNM Classification |
| I | T1, N0, M0 |
| IA | T1a, N0, M0 |
| IB | T1b, N0, M0 |
| IC | T1c, N0, M0 |
| II | T2, N0, M0 |
| IIA | T2a, N0, M0 |
| IIB | T2b, N0, M0 |
| IIIA1 | T1/T2, N1, M0 |
| IIIA2 | T3a, NX/N0/N1, M0 |
| IIIB | T3b, NX/N0/N1, M0 |
| IIIC | T3c, NX/N0/N1, M0 |
| IV | Any T, Any N, M1 |
| IVA | Any T, Any N, M1a |
| IVB | Any T, Any N, M1b |


