Small Cell Lung Cancer
Survivorship
Survivorship is defined in different ways. Some people identify as a survivor at diagnosis; others consider themselves survivors once primary treatment has ended or as they start maintenance therapy. However you define it, it is important to have a conversation with your doctor about having a survivorship care plan. This plan is designed to keep track of all pertinent information about your care and may include your medical history, ongoing medications, a treatment summary and more.
Sometimes it may feel like cancer is making all the rules, but there is one way you can exert some much-needed control. Take an active role in your survivorship care plan by choosing to lead a healthy lifestyle. Draw on the support of your family, friends, health care team and trusted resources to help you move forward and make a positive impact during treatment. Ask your doctor for a plan or start one on your own.
Nutrition
Research shows that good nutrition during cancer treatment offers a better chance at recovery. However, getting the nutrients and fluids your body needs to heal can be challenging. Working with a dietitian to help tailor a nutrition plan soon after diagnosis can get you started on the right track.
Appetite loss is common during cancer treatment. It can be caused by fatigue, stress, depression, pain and treatment side effects, such as nausea, constipation and changes in how food smells and tastes. The weight you may lose is not just weight you feel you can stand to lose; it is also loss of muscle mass, so it is important to ensure you are eating the calories and nutrients your body needs. As you go through treatment, your body needs more nutrients and calories to withstand the treatment. It will be important to keep your strength up, and high protein foods may help.
Staying hydrated during treatment for SCLC is crucial. Sipping water can remedy a dry mouth, thin the mucus in your throat and feel soothing after coughing. Some treatments, such as radiation therapy, can increase your risk of dehydration, which can cause nausea, fatigue, dizziness and headaches. Side effects of certain drug therapies, such as diarrhea or vomiting, can also cause dehydration. Drinking water can help reduce that risk. However, if diarrhea is severe, you may not be able to absorb plain water, and your doctor may recommend a specialized oral rehydration solution. Talk to your doctor or dietitian for more information.
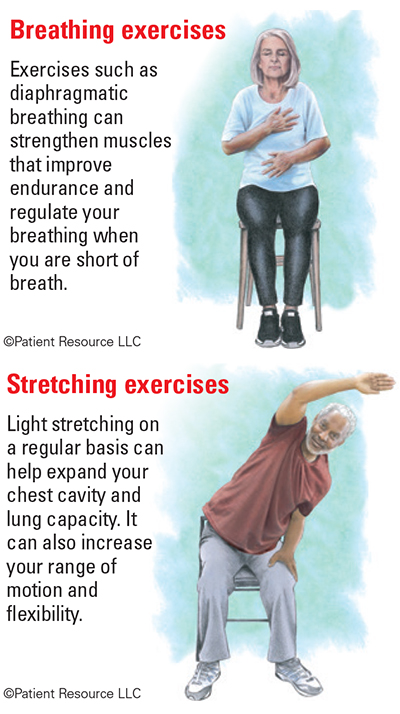
Exercises for People with Small Cell Lung Cancer
Exercise
As surprising as it may sound, exercising while you have SCLC is possible — and encouraged. The type of exercise you can do now may be different than what you are used to, but the rewards will be the same: more energy, decreased fatigue and improved mood. Feeling better overall also positions you to better manage treatment-related side effects.
Your exercise plan should be focused on avoiding inactivity and simply getting moving. Try not to be completely sedentary. Instead, set a goal to get back to the activity level you had before diagnosis. Your health care team can help tailor a daily activity plan for you that may include the following.
Breathing exercises. Performing these regularly can strengthen chest and abdominal muscles used for breathing and help you breathe easier by reducing shortness of breath (dyspnea).
Stretching. Warming up is always smart before activity. It increases blood flow and oxygen to the muscles and, in turn, increases your lung capacity. It also extends your flexibility and range of motion, and reduces stiffness.
Aerobic exercise. This is any activity that gets your heart pumping, such as dancing, swimming and biking. If those activities seem too aggressive, keep in mind that you can also get these cardiovascular benefits from walking. Being active can also help prevent and relieve constipation.
Strength training. This activity can strengthen muscles weakened by treatment and regain muscle mass. Strength training may help improve your balance and posture and increase your bone strength, which is especially important if cancer has metastasized to your bones. It may be nice for family and friends to want to do things for you but continuing daily tasks such as cooking and light chores can help prevent some muscle loss.
Sleep Hygiene
Your regular sleep pattern may be interrupted. Often, disrupted sleep can be attributed to pain and the physical and mental challenges caused by cancer, treatment or side effects.
Try to get 7 to 9 hours of sleep per night. Start a habit of going to bed at the same time and waking up at the same time. Wind down before bed. That includes shutting down your screens, such as your TV and phone, because blue light activates your brain and can keep you from falling asleep. Turn on relaxing music. Avoid snacking, drinking caffeine and exercising too late into the evening. Talk with your doctor about additional ways to get enough rest if you have trouble maintaining a good sleep schedule.
Sexual Health
Cancer and its treatment may affect how you feel about yourself and your body and how you relate intimately to your partner. Lack of desire is the most common sexuality issue among both men and women with cancer. Untreated side effects can reduce the interest in sex, libido and feelings of desirability. Talk with your doctor before treatment begins to find out what to expect in terms of sexuality issues and when it is safe to resume sexual activity after treatment.
Tobacco Use
If you currently smoke or use tobacco products, it is important to stop and to avoid smoky environments. Use the resources on this site in Treatment Planning or ask your health care provider for more information.
Get involved with the Lung Cancer Community to help bring more awareness to SCLC
- World Lung Cancer Day is always on August 1
- November is Lung Cancer Awareness Month
Your Health Care Team
From diagnosis through survivorship, these and other health care professionals may be involved in your care.
Medical oncologists treat cancer with drug therapy and other medications.
Surgical oncologists operate to remove cancer tumors and have special training in performing biopsies.
Oncology nurses provide inpatient or outpatient care in a cancer treatment facility.
Pulmonologists are doctors who have special training in diagnosing and treating diseases of the lungs.
Thoracic radiologists are experts at imaging the chest.
Thoracic surgeons operate in the chest.
Respiratory therapists are health professionals trained to evaluate and treat people who have breathing problems or other lung disorders.
Radiation oncologists treat cancer using radiation therapy.
Nurse navigators/patient navigators serve as guides throughout the continuum of care, from diagnosis through treatment and follow-up. They may also be patient advocates, helping identify barriers to treatment such as the need for transportation or help with copays and deductibles, and accessing resources to resolve such barriers.
Palliative care specialists work to provide physical and emotional relief for cancer symptoms and treatment-related side effects.
Rehabilitation specialists, including physical, occupational and speech therapists, help restore movement and build physical strength after cancer treatment.
Nutritionists/dietitians help meet nutritional challenges that arise during and after treatment.
Oncology pharmacists have special training in how to design, administer, monitor and adjust chemotherapy for cancer patients.
Pharmacists have special training in preparing and dispensing prescription drugs. They are an excellent resource for learning about the use and storage of medications, and the possible side effects and interactions with your current prescriptions and over-the-counter therapies.
Case managers/social workers assist you and your family if you need psychosocial (emotional) care or assistance, or require resources outside of medical care or advance directive planning.
Geriatric specialists are physicians who focus on the health care of elderly people.