Prostate Cancer
Diagnosing & Staging
Prostate cancers are most often first discovered as a result of a blood test for prostate-specific antigen (PSA), a protein found in the blood of men and produced primarily by normal and malignant prostate glands. Your doctor may order this blood test because a prostate problem is suspected or simply as a routine screening test. Once your doctor suspects you may have prostate cancer, additional tests will be needed to confirm a diagnosis.
Your doctor may perform any of the following tests. Some may also be used for monitoring once treatment begins.
Physical Exam
A digital rectal exam (DRE) is a test to screen for prostate cancer and to determine the size of the tumor. The doctor will insert a lubricated, gloved finger into your rectum and feel for any abnormalities in the prostate.
Blood Tests
Prostate-specific antigen (PSA) is a common biomarker test performed to look for prostate cancer. Biomarkers are substances in blood, body fluids or tissues that may indicate a condition or disease, such as cancer. Some PSA enters the bloodstream and can be measured in a small sample of blood.
Generally, higher PSA levels indicate a greater likelihood that prostate cancer cells are present. But infection, inflammation, enlargement or other injuries to the prostate can also increase a man’s PSA level. The U.S. Food and Drug Administration originally approved the test to be used in combination with a digital rectal exam (DRE), and they are often used together for screening and diagnosing prostate cancer.
A man’s PSA level may increase with age. It is important to be tested regularly so your doctor can compare these levels over time and watch for an increase, which may indicate a need for further evaluation.
Other tests may be used along with the PSA to better determine whether you have cancer and to avoid unnecessary biopsies:
- PSA density (PSAD) may be used in men with larger prostate glands. PSAD attempts to consider the fact that benign enlargement of the prostate in and of itself may increase the PSA level. A higher PSAD level may indicate a greater likelihood of cancer. It is calculated by dividing the PSA by the size of the prostate measured by ultrasound or MRI.
- PSA velocity measures how fast PSA levels change over time. A high PSA velocity (i.e., a more rapidly increasing PSA) may indicate prostate cancer and may help find fast-growing prostate cancers.
- PSA doubling time is the time it takes for the PSA level to double. It indicates how fast the cancer is growing, spread of the cancer beyond the prostate, or both, and it may be used to determine your risk for a recurrence if you have already been treated for prostate cancer.
- Percent-free PSA is a type of PSA test that measures the proportion of the total PSA that is circulating “freely” in the blood (not bound to other blood proteins). It is compared to the amount of PSA attached to other proteins. Men with benign prostatic hypertrophy (BPH) have higher amounts of free PSA.
- Prostate Health Index (PHI) measures PSA, free PSA and proPSA and uses a formula to predict the presence of prostate cancer in men with an elevated PSA level.
- 4Kscore Test measures PSA, free PSA, intact PSA and human kallikrein 2 (hK2) in a blood sample and combines these results with age, DRE and whether a man had a previous negative biopsy into an algorithm to predict the likelihood that a biopsy would show a high-grade cancer.
Urine Tests
Some biomarkers can be tested for in urine. The PCA3 test measures the level of the prostate cancer antigen 3 (PCA3) in the urine. This test may be done with PSA testing to determine whether a repeat biopsy is necessary in men who have had negative results on previous biopsies.
Biopsies
A biopsy is the only way to definitively diagnose prostate cancer. Multiple tissue samples (typically 12 to 14) are usually collected to be examined under a microscope.
- Core needle biopsy is the most commonly used test for detecting the presence of cancer in the prostate.
- Transrectal ultrasound (TRUS)-guided biopsy uses sound waves to visualize the prostate and evaluate for cancer and other conditions. The ultrasound image is also used by the doctor to guide needles to the correct areas during the biopsy.
- Transperineal ultrasound-guided biopsy removes tissue with a thin needle that is inserted through the skin between the scrotum and rectum and into the prostate.
- MRI-ultrasound fusion biopsy fuses, or combines, detailed MRI images with live, real-time ultrasound images of the prostate. An MRI is done first. At another appointment, an ultrasound of the prostate is performed. Fusion software combines the images from both tests and gives the doctor a detailed three-dimensional ultrasound/MRI view to help guide the biopsy needles more precisely to areas suspicious for cancer.
- Pelvic lymphadenectomy is a surgical procedure to remove lymph nodes in the pelvis to see whether they contain cancer. This procedure is important to determine the cancer’s stage. Lymph node removal may be done at the same time surgical removal of the prostate is performed.
- Seminal vesicle biopsy uses a needle to remove a sample of tissue from the seminal vesicles, imaged by ultrasound, to check for spread of the cancer.
Imaging Tests
Transrectal ultrasound (TRUS) uses sound waves to visualize organs. This imaging test may be used to find possible areas of cancer, assist with a biopsy, measure the size of the prostate gland and guide some forms of treatment. During this test, the technician will insert a lubricated transducer (a small instrument that emits sound waves) into the rectum. As the sound waves reach the prostate and create echoes, images of the prostate will appear on the monitor.
Magnetic resonance imaging (MRI) uses magnetic fields to visualize internal organs in the body. The MRI may be particularly helpful in showing a detailed view of the prostate.
Multiparametric MRI (mpMRI) may be used to find possible areas of cancer in the prostate. mpMRI employs injection of contrast material into a vein to provide a more detailed picture of the prostate. This procedure provides more sensitive information regarding a cancer and allows the physician to gain some information about the aggressiveness of the tumor, such as how quickly it may grow and the risk the cancer has grown outside the prostate or spread to other organs.
A bone scan may be performed to determine whether cancer has spread to the bones.
Computed tomography (CT) is primarily performed to look for the spread of cancer to lymph nodes and other organs but is not especially helpful at showing details inside the prostate.
Positron emission tomography (PET) involves intravenous administration of a tiny dose of radioactivity to identify whether the cancer has spread. A new version of PET, the PSMA PET, attaches to prostate-specific membrane antigen (PSMA), a protein found in prostate cancer cells.
Such a scan is called ProstaScint scan and it detects the presence of PSMA on the surface of prostate cancer cells using an antibody carrying a radioactive molecule that can be detected by single photon emission computed tomography (SPECT).
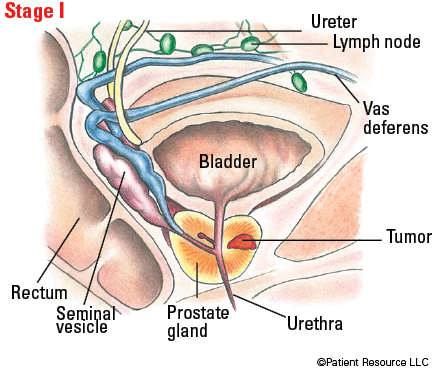
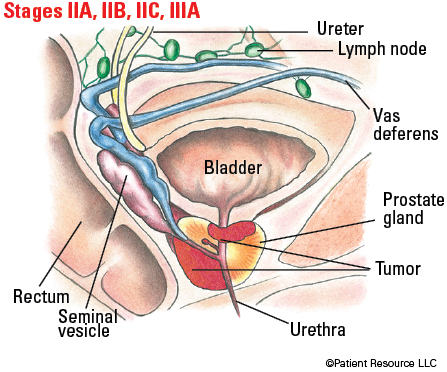
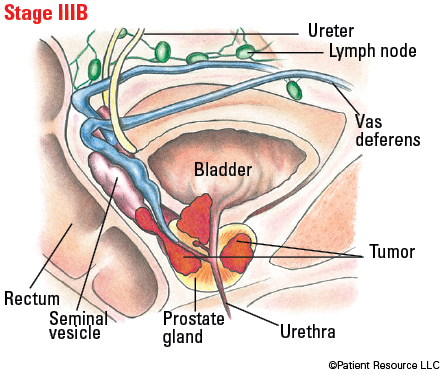
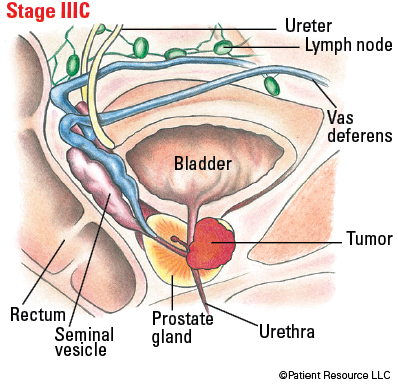
Staging and Grading Prostate Cancer
Test results are used to stage the cancer. Then the cancer is given a grade, which is how abnormal the cancer cells look under a microscope.
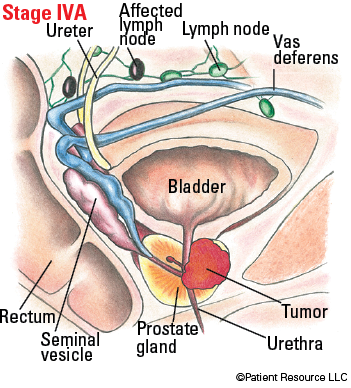
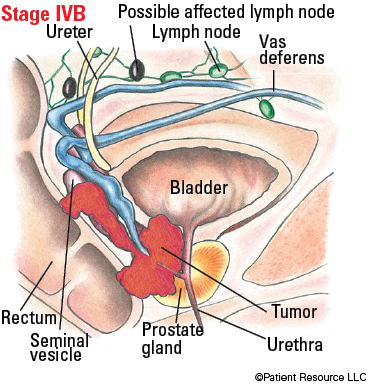
The TNM system from the American Joint Committee on Cancer (AJCC) is the staging system used to classify and stage prostate cancer. The tumor (T) is categorized by its size, including how much of the prostate is occupied by cancer and whether it has spread to adjacent structures such as the seminal vesicles, rectum, bladder and/or pelvic wall; whether cancer has affected nearby lymph nodes (N); and whether the cancer has metastasized (M), or spread, to other parts of the body.
Prostate cancers are graded from 3 to 5 using the Gleason scoring system, based on how different the cancerous cells appear from normal, healthy cells. A pathologist examines biopsied tissue containing cancer in areas that make up the largest portion of cancer cells, assigning a Gleason score to cancer cells in this area. Then the Gleason score of the second largest area of cancer is determined. The final Gleason score is the sum of these two numbers expressed as the total and component scores (such as 4+3=7). The higher the Gleason grade, the more aggressive the tumor is and the more likely it is to spread.
Table 1. TNM system for classifying prostate cancer
| Classification | Definition |
| Tumor (T) | |
| TX | Primary tumor cannot be assessed. |
| T0 | No evidence of primary tumor. |
| T1 | Clinically inapparent (produces no signs or symptoms) tumor that is not palpable (noticeable by touch). |
| T1a | Tumor incidental histologic finding in 5 percent or less of tissue resected. |
| T1b | Tumor incidental histologic finding in more than 5 percent of tissue resected. |
| T1c | Tumor identified by needle biopsy found in one or both sides, but not palpable (noticeable by touch). |
| T2 | Tumor is palpable (noticeable by touch) and confined within prostate. |
| T2a | Tumor involves one-half of one side (one prostate lobe) or less. |
| T2b | Tumor involves more than one-half of one side (one prostate lobe) but not both sides (both lobes). |
| T2c | Tumor involves both sides (prostate lobes). |
| T3 | Extraprostatic tumor (tumor extends beyond the prostate gland) that is not fixed or does not invade adjacent structures. |
| T3a | Extraprostatic extension (tumor extends beyond the prostate gland) (unilateral or bilateral). |
| T3b | Tumor invades seminal vesicle(s) (gland on each side of the bladder). |
| T4 | Tumor is fixed or invades adjacent structures other than seminal vesicles such as external sphincter, rectum, bladder, levator muscles and/or pelvic wall. |
| Node (N) | |
| NX | Regional nodes were not assessed. |
| N0 | No positive regional nodes. |
| N1 | Metastases in regional node(s). |
| Metastasis (M) | |
| M0 | No distant metastasis. |
| M1 | Distant metastasis. |
| M1a | Nonregional lymph node(s). |
| M1b | Bone(s). |
| M1c | Other site(s) with or without bone disease. |
Table 2. AJCC Prognostic Stage Groups
| Group/stage | TNM classification | Grade group | Prostate-specific antigen (PSA) level |
| I |
T1a-c, N0, M0
T2a, N0, M0 |
1
1 |
Less than 10
Less than 10 |
| IIA |
T1a-c, N0, M0
T2a, N0, M0 T2b-c, N0, M0 |
1
1 1 |
Greater than or equal to 10, but less than 20
Greater than or equal to 10, but less than 20 Less than 20 |
| IIB |
T1-2, N0, M0
|
2
|
Less than 20
|
| IIC |
T1-2, N0, M0
T1-2, N0, M0 |
3
4 |
Less than 20
Less than 20 |
| IIIA | T1-2, N0, M0 | 1-4 | Greater than or equal to 20 |
| IIIB | T3-4, N0, M0 | 1-4 | Any level |
| IIIC | Any T, N0, M0 | 5 | Any level |
| IVA |
Any T, N1, M0
|
Any grade
|
Any level
|
| IVB |
Any T, Any N, M1
|
Any grade
|
Any level
|
Illustrated Stages of Prostate Cancer