Prostate Cancer
Treatment Options
Understanding the options available to treat your prostate cancer is essential. Work closely with your medical team to learn about your choices, and have frank and honest discussions about each option and potential side effects. Learn as much as you can so you can understand your treatment plan.
Several types of prostate cancer treatment are available. To determine the treatment options that are the most appropriate for you, your doctor will consider the stage and grade of disease, and whether it has metastasized (spread), your age and overall health, results of risk assessments, predictive tests and more.
Your input at this time is important. Share your expectations for life during and after treatment, and ask about side effects, such as sexual function, fertility, and bladder and bowel control. Find out whether any are permanent or whether functionality can return. Although this is a delicate topic, do not be embarrassed. Your medical team is made up of highly skilled and compassionate professionals who are trained to help you through diagnosis and treatment.
Types of Treatment
Your doctor may recommend that you forego active treatment for the time being because treatment is not deemed necessary. If your cancer has features that indicate that it will be slow growing and unlikely to spread, treatment may be delayed or deferred. This offers the benefit of delaying side effects that accompany treatment. This may be an option when the cancer is slow growing, for much older men who are not experiencing symptoms, for men who have complicating illnesses that make therapy risky or for men with a low stage of cancer.
Watchful waiting enables your doctor to closely monitor your condition. Treatment may be given to minimize symptoms.
Active surveillance delays active treatment until test results from a digital rectal exam, PSA test, transrectal ultrasound (TRUS) or transrectal needle biopsy indicate it is time to treat. Active surveillance entails regular testing (such as PSA, DRE, TRUS or biopsy).
Your treatment plan may include one of a combination of the following local and systemic therapies.
Surgery may be used alone or with another therapy.
A radical prostatectomy removes the entire prostate, surrounding tissues and the seminal vesicles. Pelvic lymph nodes may also be removed. This surgery can be performed as open surgery, in which the prostate is removed through one large incision that can be from the belly button to the base of the penis (radical retropubic prostatectomy) or in the area between the scrotum and anus (radical perineal prostatectomy).
Minimally invasive surgery involves small incisions, robotic arms and an endoscope (robot-assisted radical prostatectomy). Minimally invasive surgery tends to result in shorter hospital stays, less blood loss, fewer surgical complications and a faster recovery time. The side effects, including erectile dysfunction and incontinence, are about the same with both types of surgery.
An orchiectomy surgically removes both testicles. It is a surgical form of hormone therapy used to reduce testosterone levels. Although not common, orchiectomy can generally be used for advanced prostate cancer that has spread.
Transurethral resection of the prostate (TURP) is a procedure designed to relieve symptoms caused by a tumor, such as a urinary blockage. TURP is not designed to cure the cancer but only to relieve obstruction to voiding.
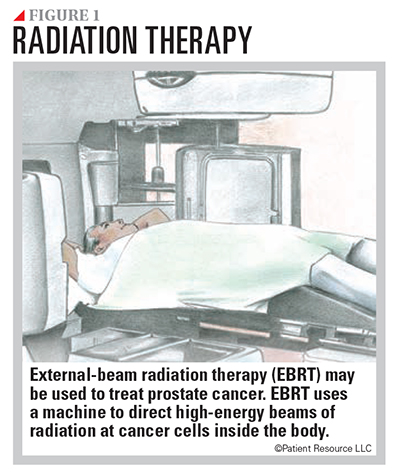
Radiation therapy may be given in an attempt to cure the cancer or after surgery to help prevent recurrence.
External-beam radiation therapy (EBRT) involves a large machine that aims radiation at the prostate and surrounding tissues (see Figure 1). High doses of radiation are focused on the cancer only, sparing healthy tissue from damage. Types of EBRT that may be used include the following:
- Stereotactic body radiation therapy (SBRT) uses high-energy radiation beams to treat cancer in fewer treatments.
- Three-dimensional conformal radiation therapy (3D-CRT) combines computed tomography (CT) images and computer software to aim beams that match the shape of the tumor.
- Intensity-modulated radiation therapy (IMRT) uses small beams of different strengths to match the shape of the tumor in the prostate and surrounding tissue.
- Proton beam radiation therapy uses streams of protons to kill tumor cells.
- Image-guided radiation therapy (IGRT) uses a computer to create a picture of the tumor that helps guide the radiation beams to ensure they target the same spot every time. It can be used with the other types of radiation.
Brachytherapy, also called internal radiation therapy, involves placing tiny radioactive “seeds,” or needles, directly into the prostate. Radiation may be delivered at a high-dose rate (over several hours) with needles implanted and removed a short time later or at a low-dose rate with small radioactive seeds that are permanently implanted. Combined with EBRT, it can also be used as a boost to treat intermediate or high-risk cancers.
Radiopharmaceuticals use a radioactive substance to treat cancer. One type is alpha emitter radiation therapy, which uses radiopharmaceuticals that are administered into the vein and travel throughout the bloodstream, delivering radiation to suppress cancer that has spread to the bones.
High-intensity focused ultrasound (HIFU) is a relatively new type of less-invasive treatment that uses high-energy sound waves to create heat to kill cancer cells. You are encouraged to find an expert in HIFU if you are considering it in your treatment plan.
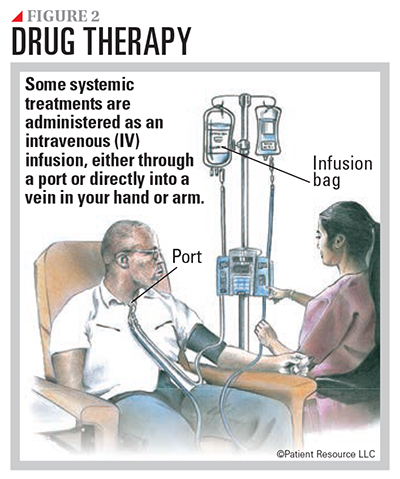
Drug therapy is systemic therapy that may be used to treat prostate cancer. Given intravenously through a vein or orally, it may be used alone or in combination (see Figure 2).
Hormone therapy adds, blocks or removes hormones. It is often used in combination with other treatments.
Androgens are male hormones. The main male androgen is testosterone, and it helps prostate cancer grow. Therefore, reducing the amount of testosterone in the body can shrink the tumor or slow its growth.
A type of hormone therapy called androgen-deprivation therapy (ADT) may slow tumor growth by preventing the body from producing androgens or by blocking the effect the androgens have on the tumor.
Given as injections or orally, luteinizing hormone-releasing hormone (LHRH) agonists and LHRH antagonists cause the testicles to stop making testosterone, a form of medical castration. Anti-androgens and androgen synthesis blockers antagonize the effects of testosterone or reduce its production from areas of the body other than the testicles. They are available as oral medications.
Orchiectomy, a surgery that removes both testicles to reduce testosterone levels, and subcapsular orchiectomy, which only removes the tissue that makes testosterone but not the covering of the testicles, are also forms of hormone therapy.
Chemotherapy uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. It also affects healthy cells (see Supportive Care). To treat prostate cancer, it may be given intravenously (IV) through a small tube inserted into a vein or port, or taken orally as a pill.
Targeted therapy, also called molecular therapy, uses drugs to target specific biomarkers found as a result of genomic testing that identifies genes, proteins or other factors that support the tumor. After considering the test results, your doctor will determine the most appropriate treatment for you. Some targeted therapy drugs are oral medications given in pill form, and others may be given intravenously by a needle inserted into a vein.
Immunotherapy is a type of therapy that uses substances to stimulate or suppress the immune system to help the body fight cancer, infection and other diseases.
Two forms of immunotherapy are approved to treat advanced prostate cancer. One is a vaccine that involves the collection of white blood cells, which are modified in a lab to recognize prostate cancer cells and then infused back into the body to find and destroy the cancer. Another is a monoclonal antibody that utilizes the body’s ability to recognize and target cancer cells that have certain biomarkers.
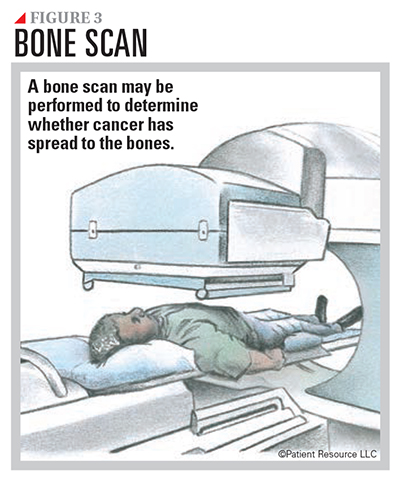
Bone-modifying (strengthening) therapy uses drugs such as bisphosphonates to strengthen bones, slow or reverse bone loss, and may help relieve bone pain. This may also reduce the risk of bone fractures.
Bone-modifying therapy may be recommended when cancer metastasizes (spreads) to the bone or if a man is receiving androgen-deprivation therapy (ADT), as ADT increases the risk of osteoporosis, a bone condition that can be caused or worsened by hormone therapy.
Your doctor may order a bone scan at diagnosis as well as during treatment to monitor bone health (see Figure 3). Damage to the jaw, a condition known as osteonecrosis of the jaw, is a serious side effect of treatment with bisphosphonates. Involve your dentist before beginning therapy if bisphosphonates are part of your treatment plan.
Medication Adherence
You may have many different medications in your treatment plan, and some of them, such as oral medications, can be taken at home. As such, you must remember that managing your cancer medications is important.
Most cancer therapies are designed to maintain a specific level of drugs in your system for a certain time based on your cancer type and stage, your overall health, previous therapies and other factors. You will get the most benefit from your medications if you take your medications exactly as your doctor intends.
Stay on track with medication adherence by doing the following:
- Talk with your pharmacist or another member of your health care team to ensure you understand how to take your medications.
- Be open and honest about any barriers you have for taking your medications, such as cost or side effects.
- Get in the habit of taking your medications at the same time every day.
- Use a pill organizer so you know whether you have taken a dose.
- Set reminders using apps, calendars, notes or timers.
PSA Persistence and Recurrence
Sometimes, even after treatment ends, cancer returns. The recurrence of prostate cancer can be detected in different ways. One indication that recurrence has happened is a measurable and increasing PSA blood level. If the PSA does not fall to or near zero after treatment, it is called PSA persistence. When the PSA level falls close to zero but subsequently rises, it is referred to as recurrence.
Recurrence or persistence of PSA will usually prompt your doctor to repeat other tests, such as a bone scan, CT or MRI. The management of recurrent or persistent PSA will depend on other types of therapy you have received and whether evidence of spread of the cancer to other organs is detected. Each of these conditions is treated uniquely. Discuss the potential treatment options with your doctor.
Clinical Trials
Clinical trials are medical research studies that evaluate treatments that involve new drugs, drug combinations, new radiation and surgical techniques, and other strategies to learn how they compare to existing treatments.
Consider discussing clinical trials and whether you may qualify for one with your doctor.
Myths vs Facts
Clinical trials are often misunderstood. Such misunderstanding may prevent people from participating in them, and this slows down progress in cancer research.
Following are some common myths and the facts that address them.
Myth: Once the clinical trial begins, you must remain in it for the duration of the trial.
Fact: Taking part in a clinical trial is voluntary, and you can leave the study at any time.
Myth: Clinical trials are only available to people who have exhausted all other treatment options.
Fact: Trials are available for all stages of cancer. Any time you or a loved one needs treatment for cancer, clinical trials might be an option to consider. Ask your doctor about clinical trials that might be an option for you.
Myth: Clinical trials are held only in large cancer centers in big cities.
Fact: Cancer clinical trials take place in doctors’ offices, clinics, cancer centers, veterans’ hospitals and other locations in cities and towns across the United States and around the world. However, you are not limited to the trials that are near you. If you choose to travel for a clinical trial but are concerned about the expenses of travel and lodging, resources may be available to help you cover the costs.
|
COMMON DRUG THERAPIES FOR PROSTATE CANCER
These therapies may be used alone or in combination. |
| Chemotherapy |
| cabazitaxel (Jevtana) |
| docetaxel (Docefrez,Taxotere) |
| mitoxantrone hydrochloride (Novantrone) |
| Hormone Therapy |
|
Androgen Synthesis Blocker
|
|
Antiandrogens
|
|
GnRH Receptor Antagonists
|
|
LHRH Agonists
|
| Immunotherapy |
| sipuleucel-T (Provenge) |
| Radiopharmaceuticals |
| lutetium Lu 177 vipivotide tetraxetan (Pluvicto) |
| radium Ra 223 dichloride (Xofigo) |
| Targeted Therapy |
| olaparib (Lynparza) |
| rucaparib (Rubraca) |
| Some Possible Combinations |
| abiraterone acetate (Zytiga) with prednisone |
| bicalutamide (Casodex) with a luteinizing hormone-releasing hormone (LHRH) analog |
| cabazitaxel (Jevtana) with prednisone |
| darolutamide (Nubeqa) with docetaxel |
| docetaxel (Docefrez, Taxotere) with prednisone |
| flutamide (Eulexin) with a luteinizing hormone-releasing hormone (LHRH) analog |
| goserelin acetate implant (Zoladex) with flutamide (Eulexin) |
| mitoxantrone hydrochloride (Novantrone) with corticosteroids |
| nilutamide (Nilandron) with surgical castration |
| niraparib and abiraterone acetate (Akeega) with prednisone |
| olaparib (Lynparza) with abiraterone and prednisone |
| talazoparib (Talzenna) with enzalutamide (Xtandi) |
As of 8/15/23
Explaining castration-resistant prostate cancer (CRPC)
Prostate cancer that continues to grow even when the amount of testosterone in the body is reduced to very low levels by medical or surgical treatment is called castration-resistant prostate cancer (CRPC).
CRPC is defined by a rising PSA level and/or worsening symptoms and/or growing cancer verified by scans. If the cancer has not spread to other parts of the body, it is known as non-metastatic CRPC. CRPC that is no longer stopped by low testosterone levels and has spread to other parts of the body is called metastatic castration-resistant prostate cancer. It is also defined by a rising PSA level and/or worsening symptoms and/or growing cancer verified by scans.
If you develop CRPC, talk with your doctor about your goals of treatment. Discuss the potential side effects of a new treatment strategy and how that fits in with your life.
Treatment for non-metastatic CRPC includes continuing to lower testosterone levels with drug therapy, generally hormone therapy or chemotherapy. The type of drug used will depend on your previous treatments and the risk of the cancer metastasizing (spreading). Surgery, such as orchiectomy to permanently stop the production of testosterone, may also be an option.
Various strategies to treat metastatic CRPC may include drug therapies, such as hormone therapy, targeted therapy, immunotherapy and radiopharmaceuticals. Bone-modifying (strengthening) drugs may also be prescribed. This may be a good time to talk with your doctor about participating in a clinical trial.
Talk with your doctor about a regular follow-up schedule to help monitor your condition. Non-metastatic CRPC will be monitored using PSA testing and/or imaging tests, such as bone scans, CT or MRI, to detect spread as soon as it occurs. The frequency of these tests will depend on the risk of metastasis. For metastatic CRPC, regularly scheduled PSA testing is common, and imaging tests will be performed when symptoms or signs indicate that the cancer is spreading.