Overview
One of the most common concerns with cancer treatment is the potential side effects. Fortunately, the advances made recently in treating many types of cancer also offer better ways of managing the variety of physical and emotional side effects that accompany a diagnosis. Rest assured that more services are now available to provide care for the whole person instead of just the disease.
Most cancer treatments have side effects that vary depending on the specific therapies (see Table 1). How you respond to those side effects, however, will depend on many factors, including your diagnosis, health history, age and other characteristics. To ease your concerns about how you will respond, educate yourself about the types of treatments in your treatment plan. Talk with your health care team in advance to prepare for possible side effects, gauge their severity and recognize what to do if they occur. Ideally, your team may help you prevent side effects from occurring or at least diminish their severity.
In addition, make your treatment team aware of your life goals before starting treatment. And, consider future life goals as well. Don’t let cancer rob you of your desires — it doesn’t deserve it and neither do you.
Being a proactive patient allows you to be an informed partner in your care, which can lead to an improved quality of life. You will be ready to manage side effects when you do your research, prepare for medical appointments, trust your instincts, take care of yourself, track your side effects, accept support and understand your medications. Ask whether telehealth appointments or an online portal are available, which may be easy ways to report symptoms or complications between follow-up visits.
Do not be afraid to report side effects. Some people worry they will be taken off their drug or the dosage will be reduced. Others hesitate to “bother” their medical team by calling. Your symptoms are important and the sooner you call, text or email the medical team, the sooner you can get your side effects managed.
You are encouraged to keep a summary of your treatment plan with you to share with any health care providers you may encounter who are unfamiliar with your situation, especially during an emergency. Additional information to have includes your exact diagnosis, the specific treatments you are taking and any known biomarkers, the names and phone numbers of your health care provider and other members of your health care team, the cancer center where you are being treated, and the address to the web portal. You can even include nearby hospitals to go to in an emergency if you’re being treated in another state. In an emergency situation, more information is better.
It is important to know you are not alone. People facing cancer have access to services that are designed to help improve their overall well-being before, during and after treatment. These services are known as palliative care. Though often confused with hospice care, palliative care has different goals. Hospice care is used for patients with terminal cancer and usually starts toward the end of life. Palliative care is actually quality-of-life preservation or restoration and focuses on symptom management associated with the cancer itself and side effects caused by treatment. Palliative care resources help with side effects, nutrition, fitness, spirituality, finances and more.
Potentially Severe Side Effects
The advances being made in treating cancer are impressive, enabling medical professionals to continue to manage and cure more types of cancer. However, to do so, they may use powerful drug therapies that are often accompanied by side effects. Some can become serious, with the potential to be life-threatening. Such side effects are sometimes referred to as adverse events. Learn as much as you can about your diagnosis and your treatment plan so you can help reduce the risk – and benefit the most – from these aggressive therapies.
If your treatment plan includes a drug therapy that has the potential for an adverse event, or severe side effect, your health care provider will talk with you about the signs and symptoms to watch for, how to identify them and which require emergency care. Make sure you and a caregiver staying with you know whom to contact and how, especially after hours. Keep the lines of communication open, and do not hesitate to reach out immediately if you experience any symptoms. Prompt treatment is necessary to keep these conditions from becoming life-threatening.
It is important to know that not all potentially severe side effects are ones you can recognize. Some are identified with lab work and imaging results, so it is crucial to stay on schedule with monitoring at your follow-up appointments.
Following are some of the most common potentially severe side effects of cancer treatments, and Table 1 details the body systems that may be affected by certain drugs, along with the adverse effects and symptoms.
- Infection can occur as a result of a low white blood cell count (neutropenia) or other factors. Contact your doctor immediately – do not wait until the next day – if you have any of these symptoms: oral temperature over 100.4° F, chills or sweating; body aches, chills and fatigue with or without fever; coughing, shortness of breath or painful breathing; abdominal pain; sore throat; mouth sores; painful, swollen or reddened skin; pus or drainage from an open cut or sore; pain or burning during urination; pain or sores around the anus; or vaginal discharge or itching. If you cannot reach your doctor, go to the emergency room. See more here.
- Immune-related adverse events (irAEs) may occur with certain immunotherapy drugs if the immune system becomes overstimulated by treatment and causes inflammation in one or more organ or system in the body. Some irAEs can develop rapidly, becoming severe and even life-threatening without immediate medical attention. See more here.
- Cytokine release syndrome can occur if immune cells affected by treatment rapidly release large amounts of cytokines into the bloodstream. Symptoms may include headache, fever, nausea, rash, low blood pressure, rapid heartbeat and difficulty breathing. See more here.
- Infusion-related reactions most frequently occur with treatment given intravenously (IV) through a vein in your arm, usually soon after exposure to the drug. Reactions are generally mild, such as itching, rash or fever. More serious symptoms, such as shaking, chills, low blood pressure, dizziness, breathing difficulties or irregular heartbeat, can be serious or even fatal without medical intervention. See more here.
- Tumor lysis syndrome (TLS) may occur after the treatment of a fast-growing cancer, especially certain blood cancers. Symptoms may include vomiting, diarrhea, muscle cramps or twitches, neuropathy and decreased urination. TLS can potentially cause damage to the kidneys, heart, liver or other organs. See more here.
Common Physical Side Effects
Although most cancer treatments have side effects, it may comfort you to know that advances in research have made it possible to minimize and even prevent some of them. The key is communication.
As you talk about your treatment options with your health care provider, discuss the potential side effects of each option so you consider them based on your expectations for your quality of life. Ask how to recognize symptoms and when to expect them. Make sure you know what to do if a side effect occurs and when to seek medical attention.
Continue to update your health care team between your follow-up appointments about your symptoms, including when they occur, how they make you feel and whether anything relieves them. You can download a free tracker at PatientResource.com/Tracker to help you remember the details. Addressing side effects early is important because when you feel better, you will be more likely to stay on your treatment plan.
This section contains some of the most common side effects of cancer treatment.
Focus on Maintaining a Healthy State of Mind
A cancer diagnosis affects more than just your body. It also affects your emotional well-being, making it important to take advantage of the various supportive care services available. Support is accessible in many forms, both in person and online. Some organizations offer one-on-one buddy programs that pair you with another person who has the same type of cancer as you. It can be very impactful to share your feelings with others who can relate because they have been through something similar.
Following are some emotions you may experience and suggestions for ways to feel better.
Anxiety can be feelings of fear, dread and uneasiness that may occur as a reaction to stress. A person with anxiety may sweat, feel restless and tense, and have a rapid heartbeat. Anxiety can begin as soon as you receive your diagnosis. Moderate to severe anxiety is often treated with medication, therapy or a combination of both. Explore relaxation techniques, such as meditation, muscle relaxation, yoga or guided imagery.
Depression is a mental condition marked by ongoing feelings of sadness, despair, loss of energy, and difficulty dealing with normal daily life. Other symptoms include feelings of worthlessness and hopelessness, loss of pleasure in activities, changes in eating or sleeping habits, and thoughts of death or suicide. Depression can occur at any time during treatment. Before treatment, if possible, talk to your health care provider about the risk of depression occurring as a side effect of your prescribed treatment.
As a side effect of medication or the result of low hormones, depression is a physical reaction resulting from chemical imbalances in the brain — specifically, decreases in the levels of serotonin and norepinephrine, chemicals that regulate moods.
Certain ongoing treatments, such as chemotherapy or hormone therapy, can cause or contribute to depression. Don’t avoid talking to your health care provider about it because you think depression is just part of having cancer — it isn’t. Call your health care provider’s office if you have 5 or more symptoms of depression that last for 2 weeks. If you feel hopeless, helpless or numb for more than a few days or have thoughts of death or of attempting suicide, seek medical attention immediately.
Distress is an unpleasant emotion, feeling, thought, condition or behavior. People with cancer may have trouble coping with their diagnosis, physical symptoms or treatment. It is normal to experience some amount of distress when you have cancer, but when it interferes with treatment, makes it difficult for you to function or cope, or affects all parts of your life, talk with your health care provider.
Doubt can lead to confusion and questions about life and its purpose. Some people find strength in support from family, friends or spirituality. It may help to open up to a counselor or support group. You may also experience doubt about your treatment decisions. Getting a second opinion can provide reassurance that you are on the right track.
Fear is common. Making plans may become difficult because every ache and pain triggers a concern. Do your best to stay focused on the present.
Guilt may occur if you feel you’ve been a burden to loved ones or if you wonder why you survived when others with similar conditions didn’t. Talk with a therapist about these feelings. You might find that you can lessen your guilt by giving back to the cancer community. Helping others may provide a sense of purpose and well-being that takes away some of the blame you place on yourself.
Scanxiety describes the anxiety that can happen when you are awaiting results from imaging scans or laboratory tests. You may feel anxious as the appointment nears and stay that way until you get your results. These suggestions may help manage the stress:
- Set expectations with your medical team about when and how you will receive the results so you are not left waiting and wondering.
- Occupy your mind with things you enjoy. Staying busy gives you less time to worry.
- Try to calm your nerves with meditation or deep breathing.
Be Open to Support
Supportive care services can connect you with resources to help you work through your feelings. These suggestions may also be helpful.
- Allow yourself to fully express your emotions when they occur to help you avoid releasing bottled-up feelings in unhealthy ways.
- Ask about cancer support groups available in your community, options for online support or phone-based peer support programs. Cancer survivors can be a great source of support, friendship and insight.
- Explore meditation, gentle yoga, massage therapy, deep breathing exercises or other relaxation techniques.
- Get outside, regardless of the season. Fresh air and nature can be therapeutic.
- Express your feelings by writing in a journal.
- Take charge of things you can control. If decision-making feels overwhelming, ask loved ones to handle routine decisions for now.
- Give yourself permission to grieve the loss of the life you had before cancer. Consider setting some new life goals to achieve after treatment is completed. This is a life-altering experience but also can be life-changing for the better for many people.
- Staying positive is important, but give yourself a break when you need it.
- Find something to laugh about every day.
- It’s extremely important to talk with your health care provider about feeling depressed, hopeless or desperate, particularly if these feelings last more than a few days. Seek medical attention immediately for thoughts of suicide.
More Areas of Support
Having cancer can affect many parts of your life, and other types of support are available to ensure your whole person is being cared for. If you are having challenges in an area not listed here, talk with your health care team. You do not have to go through this alone.
Social support is available in many forms, both in person and online. Family and friends are wonderful resources, but they can only understand so much. Find a support group for cancer survivors online or in your area. Many organizations offer one-on-one buddy programs that pair you with another person who has the same type of cancer as you. Opening up to people who have had a similar experience can offer comfort and support that is invaluable. Consider contacting a counselor and therapist with expertise in working with people living with cancer.
Dietary support may be needed if you have challenges eating or with your appetite. Ask your health care team for a referral to a dietitian who can help you understand how to get the nutrients your body needs.
Spiritual or religious guidance may be available from a chaplain or spiritual care advisor at the hospital or in your religious community. Spiritual support is available to you even if you do not consider yourself a religious person.
Financial counseling is accessible from a social worker, nurse navigator or financial counselor. The stress and anxiety of paying for treatment and other related expenses can negatively affect your well-being. Understanding the costs ahead can help you feel more in control.
| Treatment Type | Side Effect* |
| Chemotherapy | Anemia, appetite loss, blood disorders, bone loss, cardiotoxicity (heart problems), cognitive dysfunction (memory problems), constipation, diarrhea, fatigue, fertility issues, hair loss, mouth sores, nausea and vomiting, nervous system effects, neutropenia, pain, skin and nail changes, weight changes |
| Hormone Therapy | Cognitive dysfunction (memory problems); deteriorating bone health; fatigue; gastrointestinal symptoms; higher risk for other health issues including blood clots, cataracts, heart attacks and strokes; hot flashes and night sweats; infertility; mood changes; sexual health concerns; vaginal and menstruation changes (in women) |
| Immunotherapy | Anemia, bone marrow suppression, breathing problems, constipation, cough, cytokine release syndrome (CRS), diarrhea, eye problems, fatigue, fertility issues, fever, gastrointestinal problems, immune effector cell-associated neurotoxicity syndrome (ICANS), immune-related adverse events (irAEs), infections, infusion reactions, kidney problems, lower blood counts, muscle and joint pain, neuropathy, skin reactions |
| Radiation Therapy | The location of the tissues that are being radiated greatly influences what side effects may occur with the exception of fatigue, which happens for most people. Bone loss, cardiotoxicity (heart problems), cough, diarrhea, difficulty swallowing, dry mouth, extreme fatigue, fever, hair loss (in the area of the body being treated), headache, incontinence, lymphedema, mouth sores, nausea and vomiting (if abdomen is radiated), rectal bleeding, sexual and fertility problems (if pelvis is radiated), shortness of breath (if chest is radiated), skin sensitivity, tooth decay (if the head or neck is radiated). |
| Stem cell Transplantation | Anemia, appetite loss, blood clots (thrombocytopenia), diarrhea, fatigue, Graft-versus-Host Disease, hair loss, infections, mouth sores, nausea and vomiting, taste changes, weight loss |
| Surgery | Body image changes, bruising, constipation, drainage, fertility issues, limited mobility, lymphedema, numbness, pain, slow digestion, swelling |
| Targeted Therapy | Acne-like rash, blood clots (thrombocytopenia), cardiotoxicity (heart problems), constipation, diarrhea, dry or itchy skin, fatigue, flu-like syndrome, increased risk of infection, mouth sores, nausea and vomiting, neutropenia |
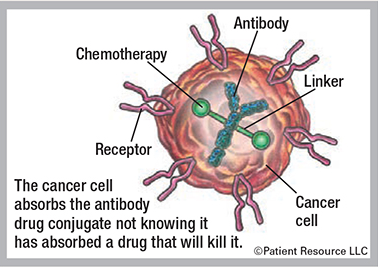
Understanding how targeted therapy works
Targeted therapy is a personalized systemic drug strategy that uses the results from genomic and biomarker testing to select a drug therapy that targets specific genes, receptors, proteins, mutations, abnormalities or other factors that are involved in the development and support of the tumor. They attack cancer in different ways.
Small molecule drugs are able to get inside a cell and target its internal components. These drugs can target the cancer’s gene expression, enzymes that affect the tumor, or certain proteins.
Angiogenesis inhibitors block new blood vessel growth that feeds tumor cells. Tumors need a blood supply to survive and grow. Without it, the tumor cells cannot survive.
Monoclonal antibodies (mAbs) are laboratory-made antibodies designed to target specific tumor antigens, which are substances on tumor cells that cause an immune response. They can flag targeted cancer cells for destruction, block growth signals and receptors, and deliver other therapeutic agents directly to targeted cancer cells.
Different types of mAbs include the following:
Naked mAbs work by themselves. No drugs or radioactive particles are attached.
Conjugated mAbs have a chemotherapy drug or a radioactive particle attached to them. They deliver treatment to the cancer cells. Types include radiolabeled antibodies, which deliver radioactive particles, and antibody-drug conjugates, which deliver a chemotherapy drug (see Figure 1).
They attach to specific receptors or proteins on the cancer cell, get swallowed by the tumor cell and break down inside the cell, releasing the toxin and causing cell death.
Bispecific mAbs are made up of two different mAbs (see Figure 2). They can be used for engaging and activating immune cells, such as T-cells, to attack a tumor, block dual signaling pathways, block immune checkpoints or form a way to replace a missing functional protein.